Medical Education: Diversity, Equity & Inclusion
Medical Education 4: Diversity, Equity, & Inclusion 1
503 - Impact of an anti-bias, anti-racism, upstander training for all staff in an large, academic, level 3 Neonatal Intensive Care Unit to reduce racial and ethnic inequities
Publication Number: 503.125

Yarden S. Fraiman, MD MPH (he/him/his)
Neonatologist
Beth Israel Deaconess Medical Center/Harvard Medical School
Boston, Massachusetts, United States
Presenting Author(s)
Background:
There are significant racial and ethnic inequities in neonatal mortality, morbidity, health outcomes, and family experience. Two potential mechanisms for health inequities are interpersonal (mediated by implicit and explicit bias) and institutional, both of which can be addressed through education, culture change, and upstander training.
Objective:
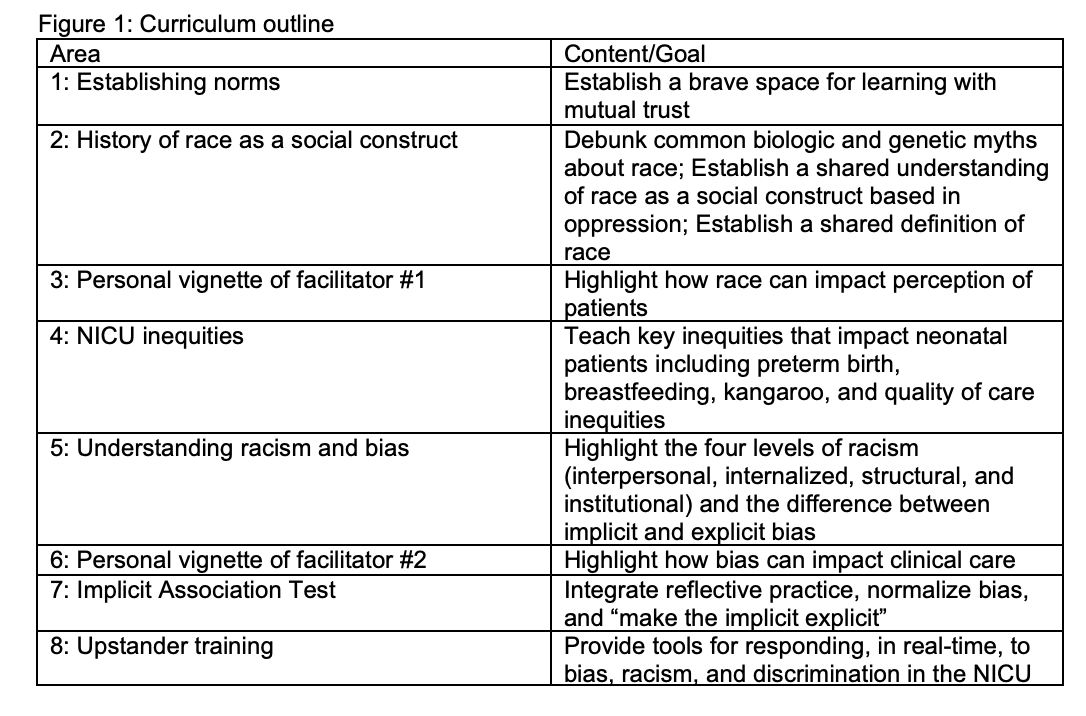
To determine the feasibility and impact of a novel, anti-bias, anti-racism, upstander training for staff administered during staff orientation. (Figure 1)
Design/Methods: We designed a one-hour lecture incorporated into a staff orientation program for a large, academic, Level 3 NICU. Anonymous, de-identified, pre- and post- surveys were administered immediately before and after the curriculum to assess (1) impact and (2) acceptability. Follow up surveys at 3 months were administered to assess long-term impact of the curriculum on knowledge and behaviors.
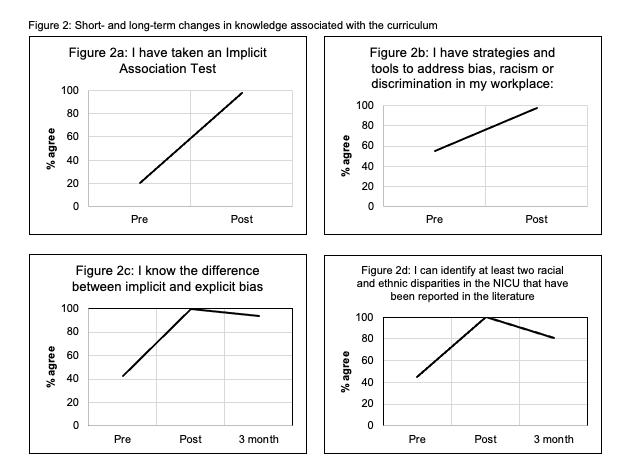
Results: Since 7/2022, 48 NICU staff members participated in the curriculum. Immediately following the curriculum, there was a significant increase in the number of participants who knew the difference between implicit and explicit bias (42.9% v. 100%), had taken an Implicit Association Test (20.4% v. 97.8%), and could identify at least 2 racial and ethnic inequities in neonatology (44.9% v. 100%). Prior to the curriculum, 55.1% endorsed having skills or tools to address bias, racism, or discrimination in the NICU which significantly increased to 97.8%. Most participants (95.5%) agreed or strongly agreed that they were comfortable using the tools learned.
After 3 months, the majority of participants continued to have persistent knowledge retention. (Figure 2) At 3 months, 73.3% agreed or strongly agreed that the IAT changed their approach with patients, and 71.4% reported using the skills learned in the education to respond to incidents of bias, racism, or discrimination.
Most participants agreed or strongly agreed that the curriculum was educational (97.8%), engaging (100%), important (100%), and would change their approach to patient care (95.6%).
Conclusion(s): A one-hour anti-bias, anti-racism, upstander training was feasible to implement and had significant impacts on short-term knowledge and led to long-term anti-racism and anti-bias knowledge-retention and upstander behaviors. This is one step in a multipronged effort to reduce neonatal health inequities. Further study is needed to understand the impact on patient experiences, particularly from minoritized backgrounds, and health inequities.