Quality Improvement/Patient Safety: Subspecialty-specific QI: see specialties above
QI 3: Subspecialty-specific QI & Patient Safety
711 - Bare Below the Elbows Practices Decrease NICU S. aureus Colonization Burden
Publication Number: 711.153
- SB
Sandhya S. Brachio, MD (she/her/hers)
Assistant Professor of Pediatrics
Columbia University Vagelos College of Physicians and Surgeons
New York, New York, United States
Presenting Author(s)
Background:
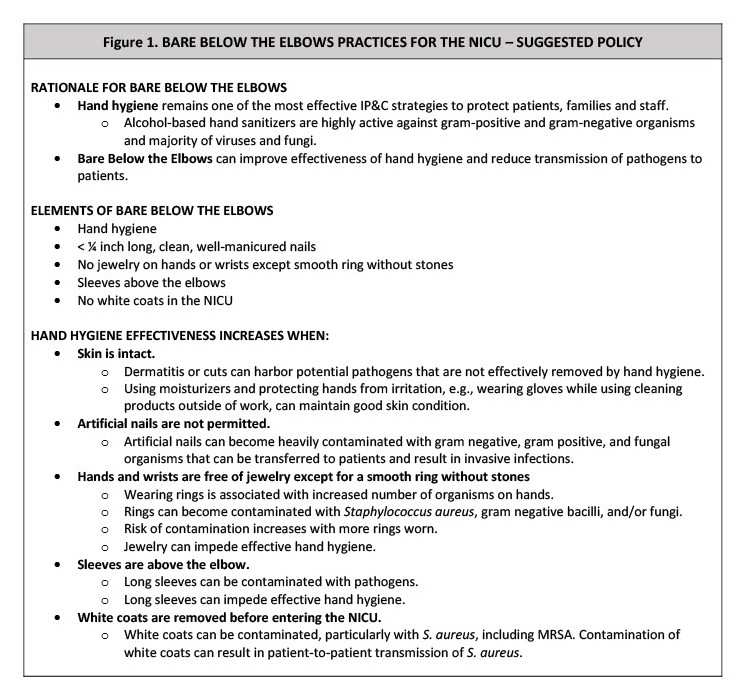
The prevalence of S. aureus (SA) infections in the NICU has ranged from 0.4-3.7% with an incidence ranging from 44.8-300 infections per 1000 infants. In addition to lower birthweight, prematurity, and invasive devices, colonization with S. aureus is an important risk factor for infection in neonates. Hand hygiene is the standard of care globally and considered the most important infection prevention and control measure to prevent hospital-acquired infections. Artificial nails, watches and rings with stones can be colonized with pathogens and impede effective hand hygiene, and long sleeves from clothes and white coats can become contaminated and lead to patient-to-patient transmission. Bare Below the Elbow (BBE) practices can reduce infection risk.
Objective:
To track methicillin-resistant and methicillin-susceptible SA (MRSA, MSSA) colonization rates and environmental pathogen burden before and after implementation of BBE practices in the NICU to assess impact on colonization burden.
Design/Methods:
Our NICU is a regional perinatal center in New York City with 58 beds dedicated to general neonatal intensive care. The majority of beds are in an open pod layout; there are four isolation rooms. Our standard practice is to obtain nasal mucosal swabs biweekly for all patients to identify MSSA and MRSA isolates. This informs cohorting and decolonization practices. In May 2022, we implemented BBE practices in the NICU (Figure 1). Key stakeholders in development of these policies included NICU physician and nursing leadership, hospital epidemiologists, and environmental services. We continued routine screening for MSSA and MRSA on a biweekly basis. We also performed environmental ATP testing, an indicator of pathogen burden, on high touch surfaces.
Results:
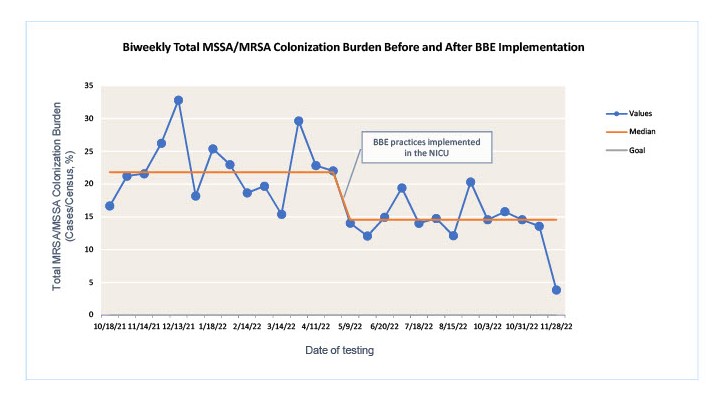
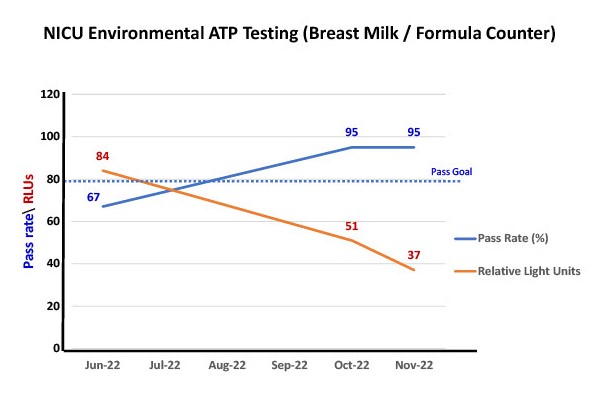
Prior to initiation of BBE practices in our NICU, Figure 2 shows a median S. aureus colonization burden of 21.8%, with 12.5 total cases of any SA and 4 new MSSA cases every two weeks. After initiation of BBE practices, we demonstrate a shift with a new median SA colonization burden of 14.5%, with 8 total SA cases and 3 new cases of MSSA every two weeks. MRSA colonization burden remained stable at 3.4%. Average daily census in the NICU was identical before and after implementation. Environmental testing revealed an improvement in pathogen burden after implementation (Figure 3).
Conclusion(s):
BBE practices in the NICU can decrease SA colonization burden in the NICU. This can be a critical infection prevention measure to reduce risk in vulnerable neonates.