Neonatal Quality Improvement
Neonatal Quality Improvement 1
656 - Implementation of a Care Bundle to Prevent Severe Intraventricular Hemorrhage in Extremely Premature Infants
Friday, April 28, 2023
5:15 PM - 7:15 PM ET
Poster Number: 656
Publication Number: 656.138
Publication Number: 656.138
Susana Arriagada, State University of New York Upstate Medical University, Syracuse, NY, United States; Swati Murthy, State University of New York Upstate Medical University, Syracuse, NY, United States; Melissa U. Nelson, State University of New York Upstate Medical University, Syracuse, NY, United States
- SA
Susana Arriagada, MD
Associate Professor of Pediatrics
State University of New York Upstate Medical University
Syracuse, New York, United States
Presenting Author(s)
Background: Severe intraventricular hemorrhage (SIVH) defined as bleeding involving more than 50% of lateral ventricles or extension into dilated ventricle (grade 3), or intraparenchymal extension (grade 4), is common in extremely preterm infants and may be associated with lifelong neurodevelopmental impairments. Therefore, SIVH prevention is of high priority.
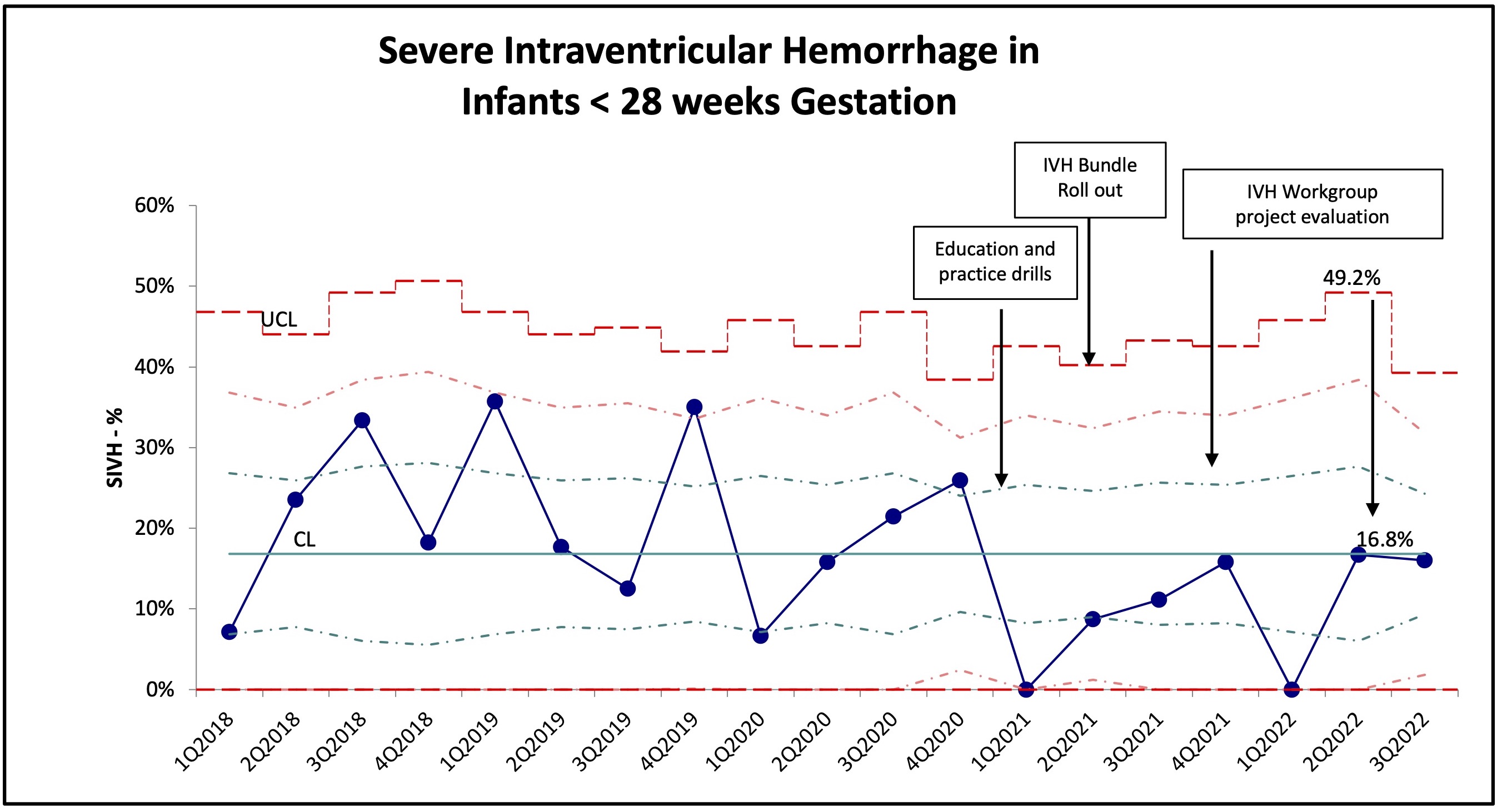
Objective: To develop and implement a standardized bundle of practices to prevent SIVH in infants born < 28 weeks gestational age (GA), with the specific aim of reducing our pre-bundle baseline incidence from 20% in 2020 to 15% within one-year post-bundle implementation (May 2021- May 2022).
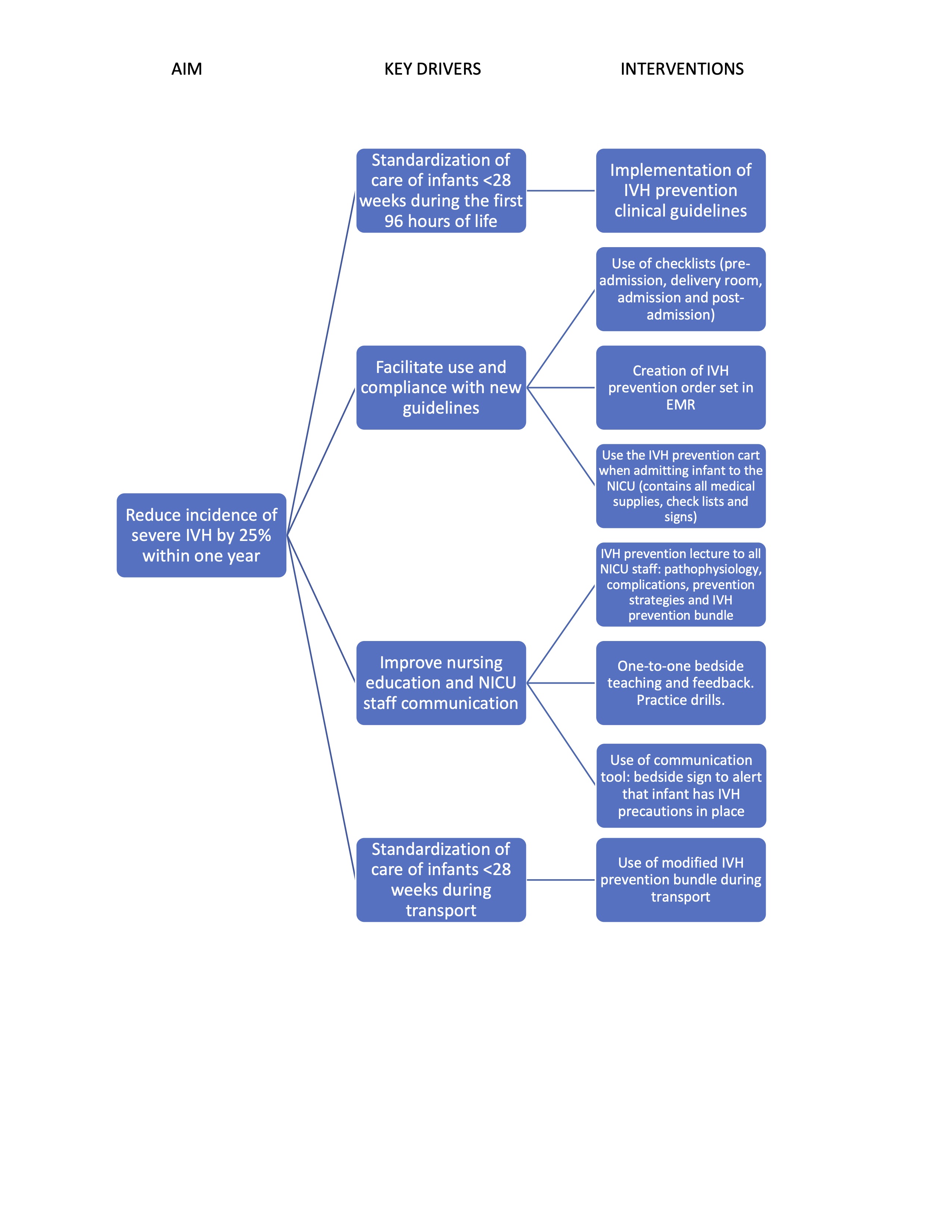
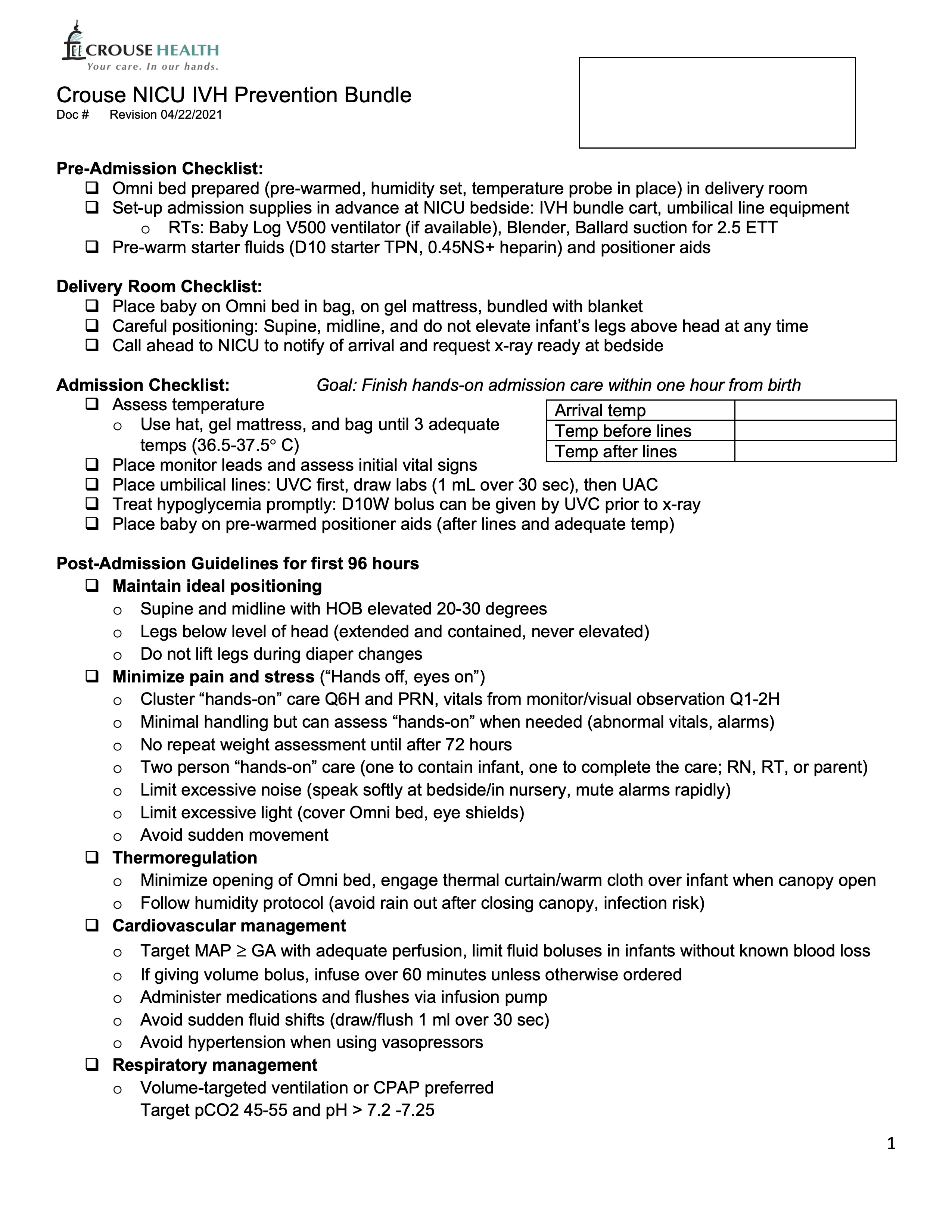
Design/Methods: A quality improvement team reviewed literature. Key drivers and interventions were identified (Fig 1) and new clinical guidelines were created (Fig 2). Guidelines addressed pre-delivery preparation, delivery room interventions, and post-admission management for the first 4 days of life. New practices focused on position supine and midline, strict thermoregulation monitoring, minimizing pain and stress, avoiding rapid intravascular fluid shifts, and preference for volume ventilation with targeted ranges of pCO2 and pH levels. Bedside nursing checklists and electronic order sets were developed. Education was accomplished with lectures, one-to-one bedside teaching and feedback, and practice drills. Plan-Do-Study-Act (PDSA) cycles were performed and process modifications were introduced in subsequent cycles. IVH was assessed with head sonogram on day of life 4 and 14 by 3 independent radiologists. The primary outcome was incidence of SIVH. Secondary outcomes were all grades of IVH and periventricular leukomalacia (PVL) assessed at 35 weeks corrected age.
Results: A total of 75 infants < 28 weeks GA born in 2020 comprised the pre-bundle group and 74 infants born from May 2021 to May 2022 the post-bundle group. The groups were similar for GA (25.3 ± 1 and 25.2 ± 1 weeks, respectively), birth weight (816 ± 211 and 760 ± 195 g) and Apgar < 5 at 5 minutes. The incidence of SIVH decreased from 20% to 11.4% (p=0.19) (Fig 3). There were no differences in other grades of intraventricular bleeds or PVL. Mortality decreased from 20% to 5.4% (p=0.012).
Conclusion(s): Standardization of care for the first 4 days of life with a bundle of potentially better practices focused on pre-delivery, delivery and post-delivery interventions was associated with a greater than 25% reduction of SIVH in infants < 28 weeks’ gestation, surpassing our goal.