Breastfeeding/Human Milk
Breastfeeding/Human Milk 1: Human Milk in the NICU
371 - An exclusive human milk diet reduces BPD, severe ROP, and surgical NEC compared to a human milk diet fortified with cow's milk derived fortifier
Publication Number: 371.101

Natalie Goldfield, MA (she/her/hers)
MD Candidate
University of Virginia School of Medicine
Charlottesville, Virginia, United States
Presenting Author(s)
Background:
Extremely premature infants are at high risk for the development of severe morbidities including bronchopulmonary dysplasia (BPD), retinopathy of prematurity (ROP) and necrotizing enterocolitis (NEC). There is ample evidence that suggests that nutrition, human milk (HM) in particular, plays in integral part in preventing these outcomes.
Objective:
To determine if a change in human milk fortifier (HMF) from cow’s milk-derived HMF (CM-HMF) to a human-milk derived HMF (HM-HMF) affects outcomes in infants ≤ 1250 grams.
Design/Methods:
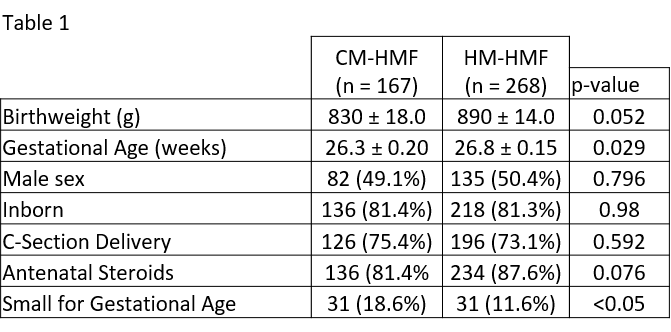
Demographical and morbidity data were collected prospectively on all infants ≤ 1250 grams birthweight between 2014 – 2020. Patients were excluded if they were admitted > 48 hours from birth or died within 48 hours after birth. Infants with congenital gastrointestinal disease were also excluded. All infants were fed a base diet of HM (either mother’s own milk or donor breast milk) and were fortified with either a liquid CM-HMF (2014-2016) or HM-HMF (2016-2020). CM-HMF infants were typically fortified to 24 kcal/oz, while HM-HMF infants were fortified to 26 kcal/oz. Per attending discretion, some infants in the HM-HMF infants were fortified to 28 or 30 kcal/oz utilizing cream. Infants were transitioned to either a preterm formula or CM-HMF at 34 weeks’ gestation (or sooner due to poor weight gain per provider discretion). Univariate analysis was performed (chi-square for dichotomous variables, student t-test for continuous variables) with an alpha of < 0.05 to determine statistical significance.
Results:
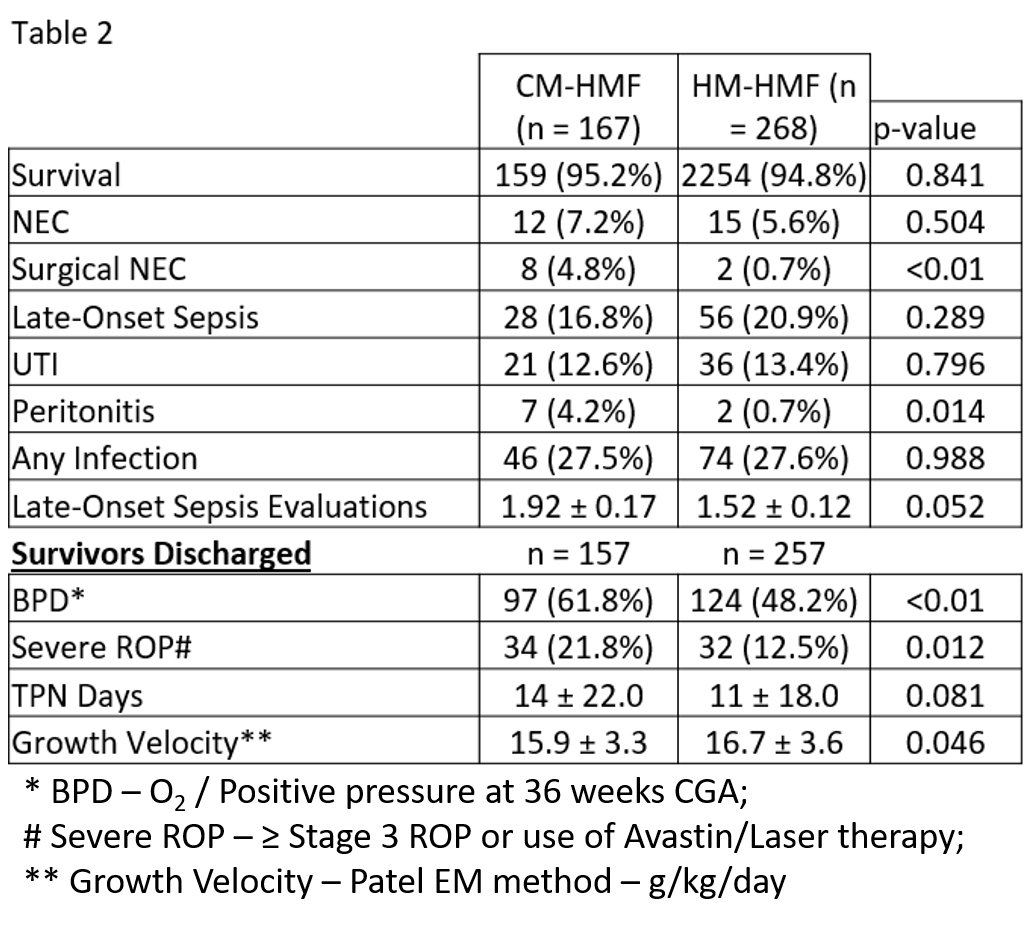
There were 167 infants in the CM-HMF cohort and 268 infants in the HM-HMF cohort. Gestational age at birth was statistically significantly lower in the CM-HMF group (26.3 v. 26.8; p=0.029), although birthweight, sex, type and location of delivery and the use of antenatal steroids were not significantly different. A higher percentage of CM-HMF infants were also small for gestational age (18.6% v. 11.6%; p< 0.05). In the HM-HMF cohort, surgical NEC (0.7% v. 4.8%; p< 0.01), BPD (48.2% v. 61.8%; p< 0.01), and severe ROP (21.8% v. 12.5%; p=0.012) were all significantly lower. Growth velocity (Patel EM method) was also higher in the HM-HMF group (16.7 g/kg/d v. 15.9 g/kg/d; p=0.046).
Conclusion(s):
An exclusive human milk diet utilizing HM-HMF, compared to a human milk diet fortified with liquid CM-HMF, can reduce significant morbidities in an extremely premature infant population. These reductions in morbidities were achieved while maintaining similar growth compared to the CM-HMF cohort. These data add to the growing literature that supports the use of an exclusive human milk diet.