Back
Background: Traditional lipid emulsions (LE) are derived from 100% soybean oil (SO) and contain high concentrations of toxic plant cholesterols, known as phytosterols (PS). Newborns receiving short-term parenteral nutrition (PN) have PS levels 2-5-fold higher than normal, while those receiving long-term PN have PS levels comparable to patients with congenital sitosterolemia ( >10 fold). PS containing LEs are a major contributor to PN associated liver disease (PNALD). Data on the cellular mechanisms by which hepatic PS accumulation affects cholesterol and bile acid (BA) metabolism is limited and conflicting. Additional mechanistic studies are needed to understand the pathogenesis of PS induced liver disease.
Objective: To determine whether PS (β-sitosterol and stigmasterol) alter the activity of sterol regulatory element-binding protein (SREBP) and affect the protein expression of key BA and sterol efflux transporters (BSEP, MRP2, and ABCG8) in human hepatocytes.
Design/Methods: SREBP activity was quantified by luciferase-based sterol regulatory element (SRE) reporter assay. DNA constructs containing wildtype SRE or non-functional mutant SRE were transiently transfected into HEPG2 cells, followed by treatment with vehicle (0.5% w/v hydroxypropyl-b-cyclodextrin), β-sitosterol (22 mM), stigmasterol (22 mM) or cholesterol (22 mM) for 48 hours in delipidated culture medium. Luciferase activity (ONE-Glo, Promega) was measured in soluble cell lysate normalized to protein concentration. BSEP, MRP2 and ABCG8 protein levels were measured by western blot in lysates prepared from native HEPG2 cells treated with sterols for 6 days. Statistical analysis was performed using ANOVA and unpaired t-test.
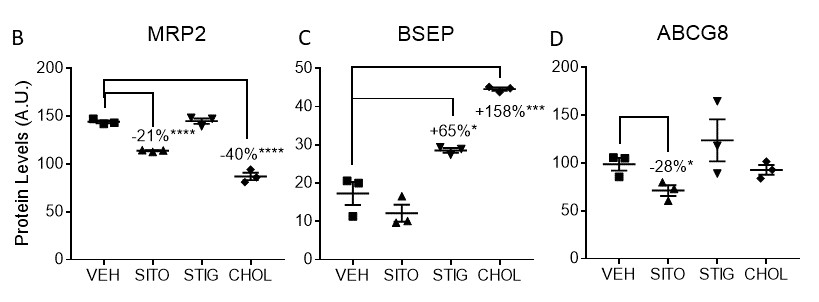
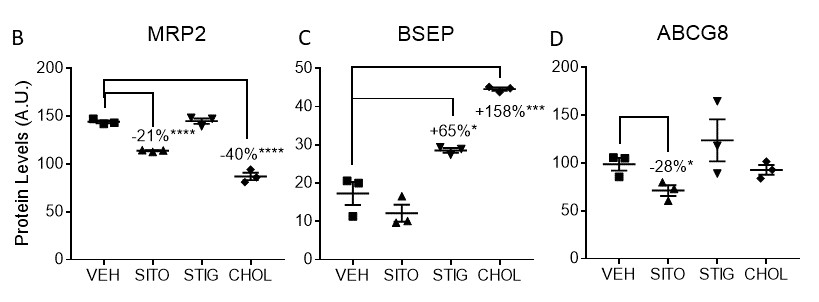
Results: Cholesterol and b-sitosterol suppressed SREBP activity by 69% and 57%, respectively, whereas stigmasterol inhibited the activity by only 20% (p< 0.0001 for each, vs. vehicle). As expected, mutant SRE reporter activity was not detectable under any condition (Fig A). MRP2 levels were reduced by b-sitosterol (-21%, p< 0.0001) and cholesterol (-40%, p< 0.0001), but not by stigmasterol. BSEP levels were increased by stigmasterol (+65%, p< 0.05) and cholesterol (+158%, p< 0.001). ABCG8 levels were reduced only by b-sitosterol (-28%, p< 0.05) (Fig B).
Conclusion(s): β-sitosterol and stigmasterol alter cholesterol homeostasis by suppressing SREBP activity and differentially alter the expression of key BA and sterol efflux transporters in human hepatocytes. These findings provide insight into various cellular mechanisms that may be implicated in the pathogenesis of PS induced liver disease.
.jpg)
Neonatal GI Physiology & NEC
Neonatal GI Physiology & NEC 2: Gut and Liver Health
355 - Phytosterols Alter Cholesterol Regulatory Pathways and Bile Acid Transporters in Human Hepatocytes
Friday, April 28, 2023
5:15 PM – 7:15 PM ET
Poster Number: 355
Publication Number: 355.134
Publication Number: 355.134
Naureen Memon, Goryeb Children's Hospital, Atlantic Health System, Morristown, NJ, United States; Elizabeth Eckman, MidAtlantic Neonatology Associates and BRInj, Cedar Knolls, NJ, United States; Aimee Herdt, Foundation for Morristown Medical Center and MidAtlantic Neonatology Associates, Morristown, NJ, United States; Chris Lee, Biomedical Research Institute of NJ, Cedar Knolls, NJ, United States

Naureen Memon, MD (she/her/hers)
Attending Neonatologist
Goryeb Children's Hospital, Atlantic Health System
Morristown, New Jersey, United States
Presenting Author(s)
Background: Traditional lipid emulsions (LE) are derived from 100% soybean oil (SO) and contain high concentrations of toxic plant cholesterols, known as phytosterols (PS). Newborns receiving short-term parenteral nutrition (PN) have PS levels 2-5-fold higher than normal, while those receiving long-term PN have PS levels comparable to patients with congenital sitosterolemia ( >10 fold). PS containing LEs are a major contributor to PN associated liver disease (PNALD). Data on the cellular mechanisms by which hepatic PS accumulation affects cholesterol and bile acid (BA) metabolism is limited and conflicting. Additional mechanistic studies are needed to understand the pathogenesis of PS induced liver disease.
Objective: To determine whether PS (β-sitosterol and stigmasterol) alter the activity of sterol regulatory element-binding protein (SREBP) and affect the protein expression of key BA and sterol efflux transporters (BSEP, MRP2, and ABCG8) in human hepatocytes.
Design/Methods: SREBP activity was quantified by luciferase-based sterol regulatory element (SRE) reporter assay. DNA constructs containing wildtype SRE or non-functional mutant SRE were transiently transfected into HEPG2 cells, followed by treatment with vehicle (0.5% w/v hydroxypropyl-b-cyclodextrin), β-sitosterol (22 mM), stigmasterol (22 mM) or cholesterol (22 mM) for 48 hours in delipidated culture medium. Luciferase activity (ONE-Glo, Promega) was measured in soluble cell lysate normalized to protein concentration. BSEP, MRP2 and ABCG8 protein levels were measured by western blot in lysates prepared from native HEPG2 cells treated with sterols for 6 days. Statistical analysis was performed using ANOVA and unpaired t-test.
Results: Cholesterol and b-sitosterol suppressed SREBP activity by 69% and 57%, respectively, whereas stigmasterol inhibited the activity by only 20% (p< 0.0001 for each, vs. vehicle). As expected, mutant SRE reporter activity was not detectable under any condition (Fig A). MRP2 levels were reduced by b-sitosterol (-21%, p< 0.0001) and cholesterol (-40%, p< 0.0001), but not by stigmasterol. BSEP levels were increased by stigmasterol (+65%, p< 0.05) and cholesterol (+158%, p< 0.001). ABCG8 levels were reduced only by b-sitosterol (-28%, p< 0.05) (Fig B).
Conclusion(s): β-sitosterol and stigmasterol alter cholesterol homeostasis by suppressing SREBP activity and differentially alter the expression of key BA and sterol efflux transporters in human hepatocytes. These findings provide insight into various cellular mechanisms that may be implicated in the pathogenesis of PS induced liver disease.
.jpg)