Back
Background: The Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) has been shown to improve food and economic security, advance health outcomes, and reduce health costs. Despite proven benefits, up to 54% of those eligible in Denver and surrounding counties are not enrolled. Barriers such as stigma, physical access, administrative resources, and psychological costs exist to enrolling and maintaining enrollment. These burdens can negatively affect health by blocking access to health-promoting programs like WIC and may have more direct health impacts from the stress of navigating burdensome bureaucracies. To lessen these barriers, Denver Health’s Federally Qualified Health Centers (FQHCs) collaborated with Denver County WIC to integrate WIC services into pediatric well-child and obstetric visits.
Objective: The aim of this analysis is to evaluate patient and provider experiences of this practice transformation work.
Design/Methods: Programmatic data were collected prior to and shortly after integrated WIC appointments using a REDCap database. The perspectives and experiences of program staff were systematically collected via interviews and surveys. Program participant feedback was gathered through surveys. Data were analyzed with descriptive statistics and inductive thematic analysis. Improvements and successes were identified.
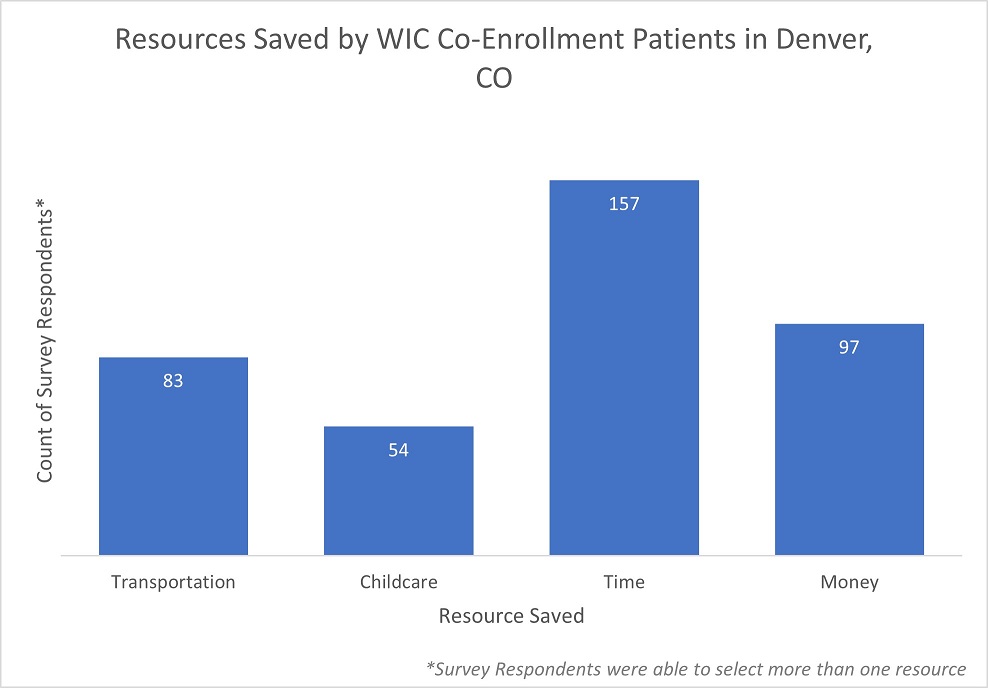
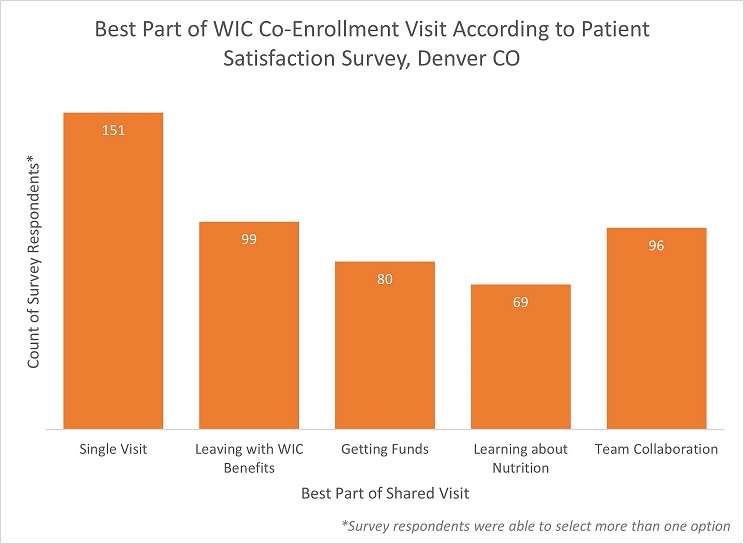
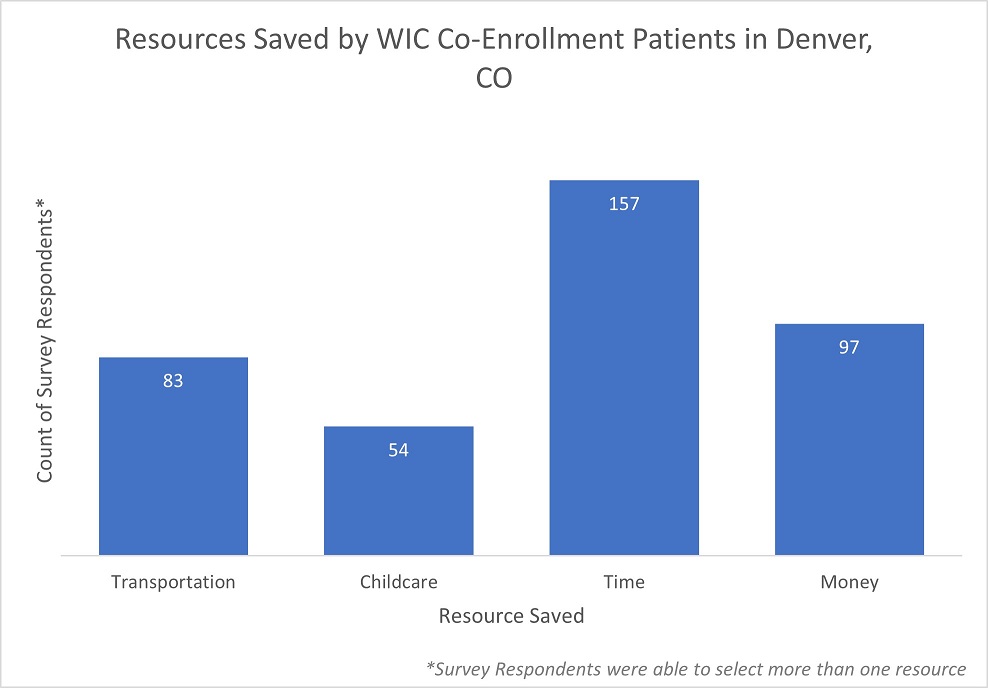
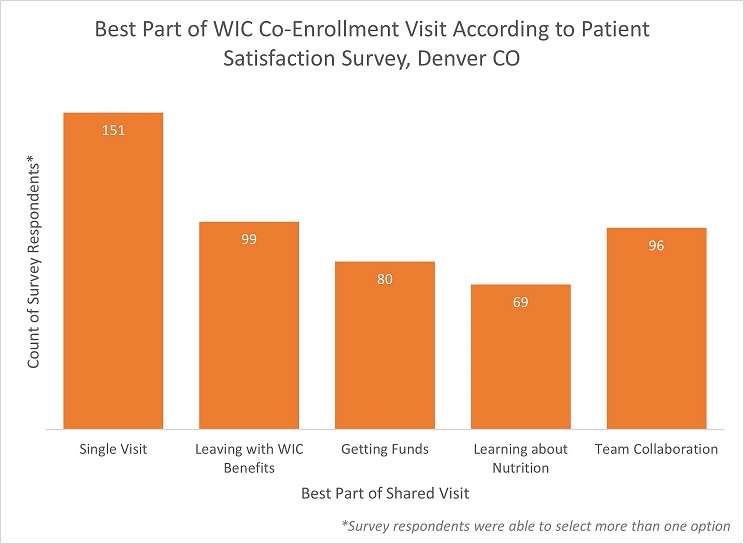
Results: Between April ‘21 and November ‘22 a total of 1,837 families were served by the integrated WIC co-enrollment program, resulting in a total of 3,291 individuals served. Of the 204 participants surveyed, almost all had positive experiences with the shared visit and noted the shared model saved time, money, and transportation resources for them and their families. Staff and providers noted convenience for patients and families as well as systemic benefits such as interprofessional collaboration.
Conclusion(s): Integrated WIC is widely popular among families, providers, and staff. Our findings suggest that the program enrolls and retains participants in a way that minimizes the administrative burden experienced by patients, minimizes downtime in the clinic setting, and improves interprofessional collaboration in primary care. Integrating WIC in primary care could be beneficial to other communities and could increase participation in this program. Integrating social safety net programs into primary care offers a family-centered model, breaking down barriers to accessing supplemental and entitlement programs. The integrated WIC program has evolved the care delivery model to one that is more collaborative and respectful of families’ time and limited resources.
General Pediatrics: Primary Care/Prevention
General Pediatrics 2
124 - WIC CoEnrollment: Evaluation of Staff and Patient Experience
Friday, April 28, 2023
5:15 PM – 7:15 PM ET
Poster Number: 124
Publication Number: 124.115
Publication Number: 124.115
Margaret M.. Tomcho, Denver Health, Denver, CO, United States; Abigail Steiner, Denver Health & Hospital Authority, Denver, CO, United States; Brittany Goldstein, Denver Health Hospital Authority, Denver, CO, United States; Jennifer W.. Moreland, Public Health Institute at Denver Health, Denver, CO, United States; Kate Bennett, Denver Health and Hospital Authority, Denver, CO, United States

Margaret M. Tomcho, MD (she/her/hers)
Medical Director for Pre-Health Programs
Denver Health
Denver, Colorado, United States
Presenting Author(s)
Background: The Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) has been shown to improve food and economic security, advance health outcomes, and reduce health costs. Despite proven benefits, up to 54% of those eligible in Denver and surrounding counties are not enrolled. Barriers such as stigma, physical access, administrative resources, and psychological costs exist to enrolling and maintaining enrollment. These burdens can negatively affect health by blocking access to health-promoting programs like WIC and may have more direct health impacts from the stress of navigating burdensome bureaucracies. To lessen these barriers, Denver Health’s Federally Qualified Health Centers (FQHCs) collaborated with Denver County WIC to integrate WIC services into pediatric well-child and obstetric visits.
Objective: The aim of this analysis is to evaluate patient and provider experiences of this practice transformation work.
Design/Methods: Programmatic data were collected prior to and shortly after integrated WIC appointments using a REDCap database. The perspectives and experiences of program staff were systematically collected via interviews and surveys. Program participant feedback was gathered through surveys. Data were analyzed with descriptive statistics and inductive thematic analysis. Improvements and successes were identified.
Results: Between April ‘21 and November ‘22 a total of 1,837 families were served by the integrated WIC co-enrollment program, resulting in a total of 3,291 individuals served. Of the 204 participants surveyed, almost all had positive experiences with the shared visit and noted the shared model saved time, money, and transportation resources for them and their families. Staff and providers noted convenience for patients and families as well as systemic benefits such as interprofessional collaboration.
Conclusion(s): Integrated WIC is widely popular among families, providers, and staff. Our findings suggest that the program enrolls and retains participants in a way that minimizes the administrative burden experienced by patients, minimizes downtime in the clinic setting, and improves interprofessional collaboration in primary care. Integrating WIC in primary care could be beneficial to other communities and could increase participation in this program. Integrating social safety net programs into primary care offers a family-centered model, breaking down barriers to accessing supplemental and entitlement programs. The integrated WIC program has evolved the care delivery model to one that is more collaborative and respectful of families’ time and limited resources.