Emergency Medicine: All Areas
Emergency Medicine 1
23 - Evaluating the proportion of low-value blood cultures obtained in a pediatric emergency department
Publication Number: 23.11
- FA
Fahd A. Ahmad, MD, MSCI (he/him/his)
Associate Professor of Pediatrics
Washington University in St. Louis
St. Louis, Missouri, United States
Presenting Author(s)
Background:
Existing literature suggests that for some pediatric conditions, blood cultures may be of low-value in specific clinical circumstances, leading to avoidable harm and costs.
Objective:
The goals of our study were: 1) identify common pediatric illnesses and define criteria for low-value blood cultures in children > 90 days of age, 2) apply these criteria retrospectively to identify the patients in our emergency department (ED) who had low-value blood cultures obtained and 3) describe this cohort and assess the proportion of true bacteremia in low-value blood cultures.
Design/Methods:
The study team consisted of two pediatric hospitalists and two pediatric emergency medicine physicians. The team reviewed the literature and developed consensus criteria to identify conditions in which blood cultures were of low-value for our study population. The criteria were applied retrospectively to well-appearing patients 91 days-18 years of age, presenting with specific diagnoses, and evaluated in our ED with a peripheral blood culture between June 2018-April 2020. Children with a central venous catheter, or who were admitted to the intensive care unit and hematology-oncology units were not included. Children with fever for 7 days or more, who were unvaccinated, immunosuppressed, had implanted devices, had a complex medical history, or had provider concerns for bacteremia were excluded. Figure 1 provides a list of diagnoses included and excluded from our study.
Results:
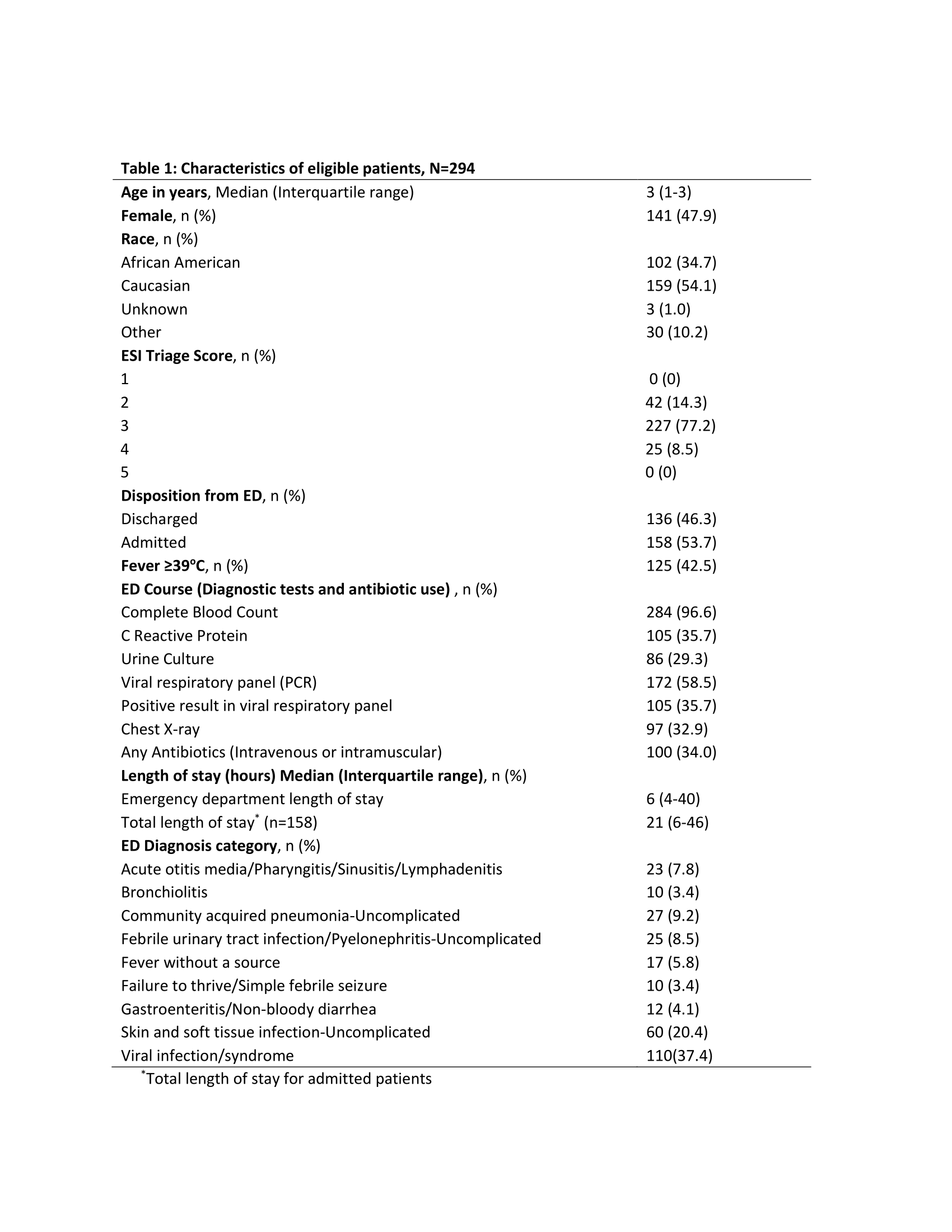
There were 1436 children potentially eligible for inclusion; after exclusions we had 294 (20.5%) patients in our cohort (Figure 2). These patients represent those who had low-value cultures per our study criteria – their characteristics are in Table 1. The most common diagnosis was viral syndrome, followed by skin and soft tissue infection (SSTI).
Nine children (9/294, 3.1%) had false positive blood cultures. The diagnoses in children with false positive cultures were viral syndrome (n=4), uncomplicated SSTI (n=2), uncomplicated community acquired pneumonia (n=2), and failure to thrive (FTT) (n=1). Three children with false positive cultures returned to the ED and were admitted, and two additional patients had repeat blood cultures.
Three patients (3/294, 1.0%) had true positive blood cultures; all were well-appearing on initial ED evaluation. Two were admitted on initial ED presentation, the third returned to the ED and was admitted, and all were discharged on oral antibiotics.
Conclusion(s): We identified a large cohort of patients in our ED who had blood cultures obtained when availabile literature indicates they were of low-value.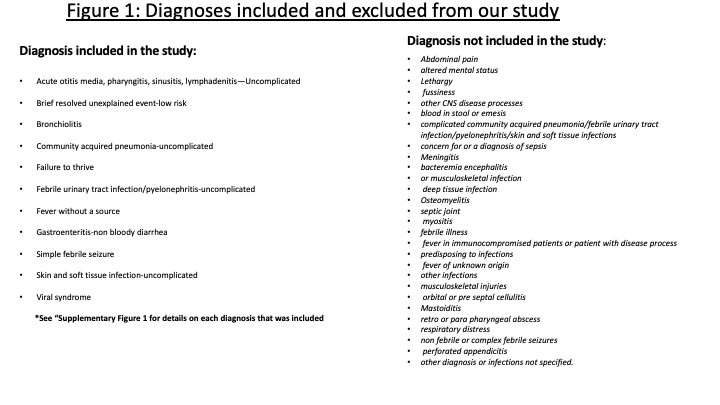
.png)
