Neonatal Quality Improvement
Neonatal Quality Improvement 2
664 - Keep the PEEP: Standardizing Early Respiratory Support in Infants <32 Weeks
Friday, April 28, 2023
5:15 PM - 7:15 PM ET
Poster Number: 664
Publication Number: 664.139
Publication Number: 664.139
Emily Sangillo, University of Maryland Children's Hospital, Baltimore, MD, United States; Katherine Nyman, University of Maryland Children's Hospital, Baltimore, MD, United States; Shruti Patel, University of Maryland School of Medicine, Baltimore, MD, United States; Erin Schofield, University of Maryland School of Medicine, Baltimore, MD, United States; Eunsung Cho, University of Maryland School of Medicine, Baltimore, MD, United States; Colleen Hughes Driscoll, University of Maryland School of Medicine, Baltimore, MD, United States

Emily Sangillo, MD (she/her/hers)
Fellow
University of Maryland Children's Hospital
Baltimore, Maryland, United States
Presenting Author(s)
Background: Infants born less than 32 weeks are at increased risk of respiratory distress syndrome due to underdeveloped pulmonary alveoli. Positive end expiratory pressure (PEEP) has shown respiratory benefits; however, our staff expressed concern that prolonged exposure to PEEP would contribute to increased risk of pneumothorax and delay initiation of oral feeding.
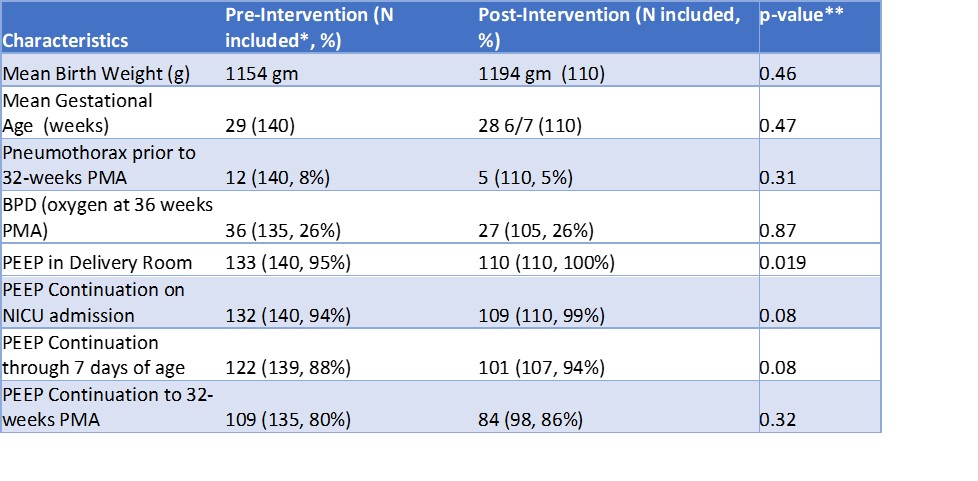
Objective: This quality improvement project aimed to increase PEEP utilization with a standardized protocol for early initiation, continuation, and subsequent weaning in infants born at less than 32 weeks gestation. We aimed to improve our PEEP initiation from 95% to 100% in the delivery room, PEEP continuation to 7 days from 88% to 95%, and PEEP continuation to 32 weeks from 80% to 90%.
Design/Methods: The current state is inconsistent use of PEEP among infants less than 32 weeks gestation that require respiratory support leading to variable respiratory support management practices. In an ideal state, clinically appropriate infants who are born less than 32 weeks gestation would be placed on PEEP until at least 32 weeks post-menstrual (PMA) with decisions to wean based upon clinical assessment, all while maintaining (or decreasing) rates of pneumothorax.
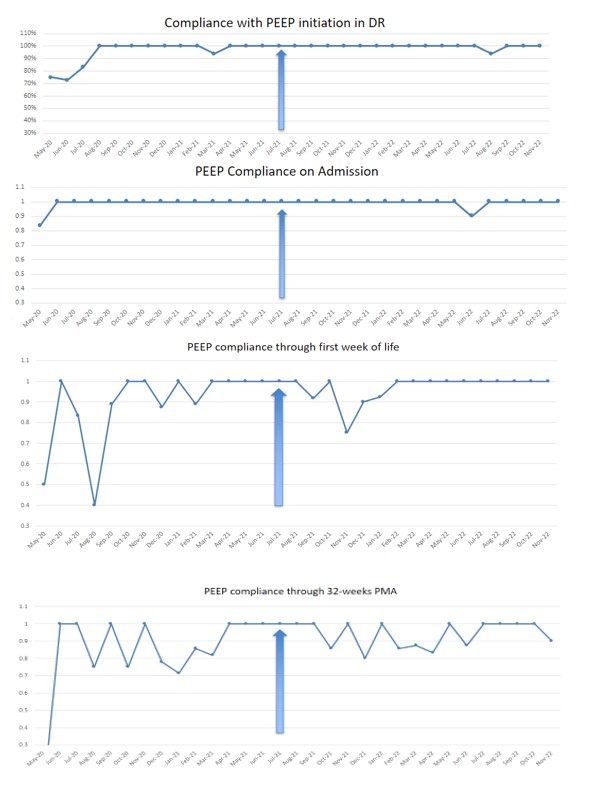
We developed a “Keep the PEEP” protocol using the Institute for Healthcare Improvement’s Quality Improvement methodology. This included initiation of PEEP at delivery, continuation through 32 weeks PMA, and guidelines for discontinuation. Data on PEEP usage were recorded between May 2020- July 2021 (baseline) and July 2021-Aug 2022 (post-intervention). Run charts were created to track compliance of our preset timelines throughout the study period. Interventions included team member training and engagement through education sessions and a poster campaign.
Results: Delivery room PEEP initiation improved from 95% to 100% following our intervention (p=0.019). There were no statistically significant differences in pneumothorax, bronchopulmonary dysplasia (BPD), PEEP continuation to NICU admission, through 7 days, nor to 32 weeks. In the post-intervention cohort, 84% had PEEP discontinued after 32 weeks PMA, and the mean gestational age at first oral feed was 34 3/7 weeks.
Conclusion(s): We successfully implemented a new respiratory protocol in our unit during the study period and improved compliance regarding PEEP usage. Despite initial concerns, adoption of prolonged PEEP use was not associated with increased incidence of pneumothoraces and initiation of oral feedings remained developmentally appropriate.