Emergency Medicine: All Areas
Emergency Medicine 3
56 - Impact of Revised Febrile Young Infant Guidelines on Emergency Department Care
Friday, April 28, 2023
5:15 PM - 7:15 PM ET
Poster Number: 56
Publication Number: 56.112
Publication Number: 56.112
Jessica M. Kelly, Childrens Hospital of Philadelphia, Philadelphia, PA, United States; Payal K. Gala, Perelman School of Medicine at the University of Pennsylvania, Mount Laurel, NJ, United States; Bobbie Hawkins, Childrens Hospital of Philadelphia, Cherry Hill, NJ, United States; Richard Scarfone, Childrens Hospital of Philadelphia, Voorhees, NJ, United States; Laura F. Sartori, Children's Hospital of Philadelphia, Philadelphia, PA, United States
.jpg)
Jessica M. Kelly, MD (she/her/hers)
Pediatric Emergency Medicine Fellow
Childrens Hospital of Philadelphia
Philadelphia, Pennsylvania, United States
Presenting Author(s)
Background: In 2021, the American Academy of Pediatrics (AAP) published guidelines for the management of infants < 60 days with fever. The impact of these recommendations, which rely on previously unused inflammatory markers (IMs) to guide clinical care, is unknown.
Objective: To compare the rates of lumbar puncture (LP) recommended by the previous clinical practice guideline (CPG) to that recommended by a revised AAP-guided CPG and to describe clinician adherence to performing LP.
Design/Methods: Retrospective cohort study of well-appearing infants 22-56 days of age undergoing evaluation for fever in the Emergency Department (ED) of a single tertiary care children’s hospital between March 26, 2022 (revised CPG publication) and September 2022. Infants met criteria for review if they had a measured temperature > 100.4º F prior to or in the ED. Infants with focal bacterial infection on exam, recent antibiotic use, or transfer from another hospital were excluded. LP recommendation using the previous CPG was compared to LP recommendation using the revised CPG for each infant. The previous CPG recommended LP for white blood cell count < 5 or >15x103/µL or band to neutrophil ratio > 0.2 in infants 29-56 days old. The revised CPG recommended LP for any abnormal IM: procalcitonin (PCT) >0.5 ng/mL, C-reactive protein (CRP) >2 mg/dL, or absolute neutrophil count (ANC) < 1000 or >4000 neutrophils/µL in infants 22-56 days old.
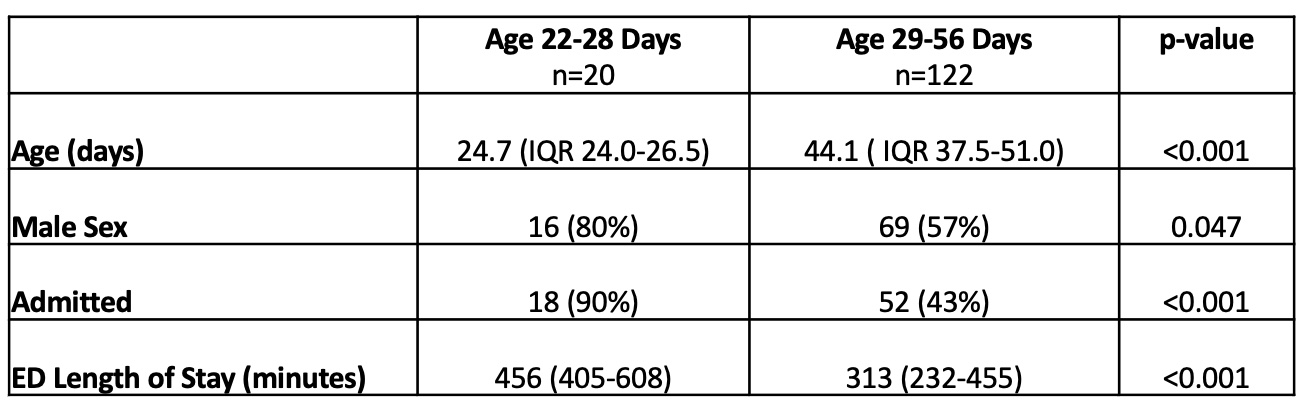
Results: 142 infants met inclusion criteria: 20 (14%) infants 22-28 days old and 122 (86%) infants 29-56 days old (Table 1). Under the previous CPG, LP was indicated in all 20 infants aged 22-28 days, but only 10 (50%) using the revised CPG (Table 2). ANC was the most frequently abnormal IM (25%), followed by CRP (20%), and PCT (15%) (Figure 1). Using the previous CPG, LP was indicated in 41 (34%) of older infants, but only 24 (20%) infants under the revised CPG (Table 2). As in younger infants, ANC was the most frequently abnormal IM (23%), followed by CRP (19%), and PCT (9%). In practice, LP was attempted in 95% of well-appearing infants aged 22-28 days and 71% of infants aged 29-56 days when LP was recommended by revised CPG. In total, 27 fewer LPs were recommended under the revised CPG. There were no missed cases of meningitis, though our study was not powered to assess this rare outcome.
Conclusion(s): Implementation of an AAP-guided CPG resulted in fewer recommended LPs, with greater clinician guideline adherence in younger infants. ANC was the most commonly abnormal IM. Future research should focus on the impact of IM abnormalities on medical decision-making.
.jpg)
.jpg)
