Neonatal Neurology: Clinical Research
Neonatal Neurology 3: Clinical 3
180 - Does acuity of injury modify the association between MRI injury severity and neurodevelopmental outcomes for neonates with Hypoxic-Ischemic Encephalopathy?
Publication Number: 180.137

Jessica L. Wisnowski, PhD (she/her/hers)
Assistant Professor of Radiology and Pediatrics Research
Children's Hospital Los Angeles
Los Angeles, California, United States
Presenting Author(s)
Background: Neonatal hypoxic-ischemic encephalopathy (HIE) is a heterogeneous disorder. The distribution of brain injury on MRI varies with the underlying cause and timing of the inciting insult. The most widely validated HIE MRI scoring systems are agnostic to the acuity of the brain injury.
Objective: The aim of this study is to determine whether the association between brain injury severity and neurodevelopmental outcome is modified by the acuity of the brain injury.
Design/Methods:
This is a posthoc secondary analysis of data from the multicenter HEAL Trial. 408 infants with moderate or severe HIE underwent MRI at < 8 days using a harmonized protocol, had outcome data available at 2-3 years of age, and were included in this analysis. MRI scans were evaluated by three experienced reviewers using a validated MRI scoring system and classified as no injury, mild, moderate or severe injury based on pre-specified cut-offs. Acute injury was defined by the presence of reduced diffusivity; subacute by MRI signal abnormalities without diffusion restriction; chronic by volume loss. The primary outcome was the 5-level ordinal outcome: alive/no neurodevelopmental disability (NDI), mild NDI, moderate NDI, severe NDI, died. Using proportional odds regression, we estimated odds ratios (OR) and corresponding 95% confidence intervals (CIs) for the associations between MRI injury severity and the 5-level ordinal outcome separately for infants with acute, subacute and acute + subacute injury.
Results:
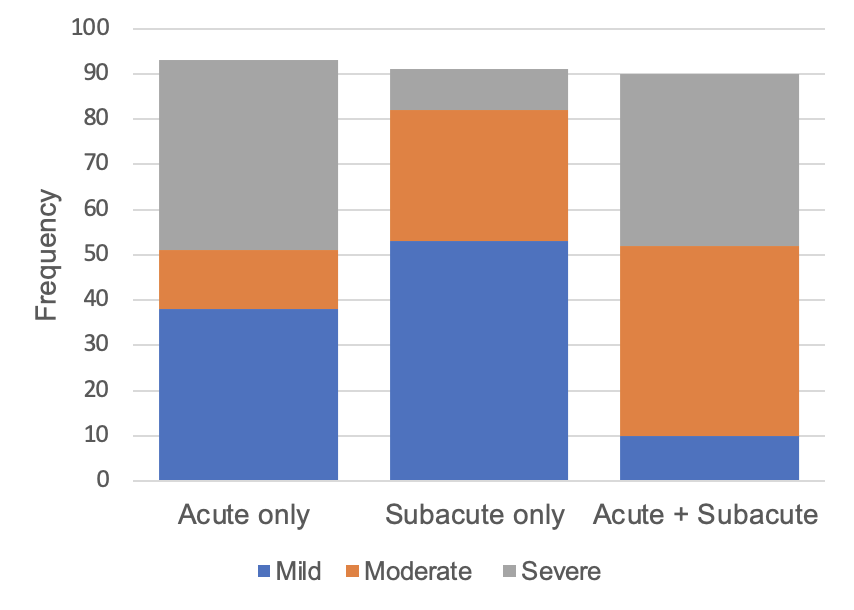
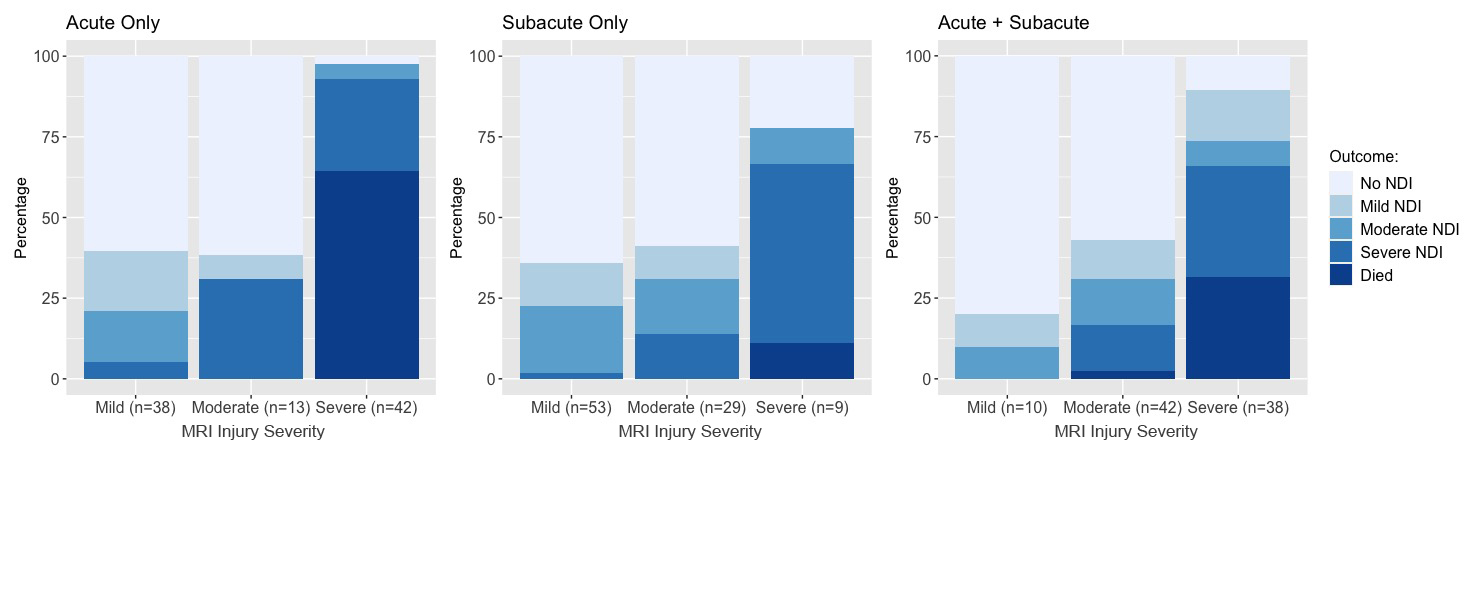
Of the 408 infants, 125 infants had normal MRIs; 93 (23%) evidenced only acute, 91 (22%) only subacute, 90 (22%) acute and subacute, and 9 (2%) chronic injuries, with similar distributions across treatment groups. The distribution of injury severity was different across acuity groups, with acute infants demonstrating bimodal distribution between mild and severe injury, and subacute and acute+subacute demonstrating skew toward mild-moderate and moderate-severe injuries, respectively (Figure 1). Increasing MRI injury severity was associated with worsening outcome with an OR of 9.18 (95% CI 4.95, 17.05) for acute injuries, 3.00 (1.58, 5.72) for subacute injuries and 7.54 (3.52, 16.14) for acute + subacute injuries (Figure 2).
Conclusion(s):
Acute, subacute and acute + subacute injuries were observed at approximately equal rates in the HEAL Trial, with variability in the distribution of injury severity by acuity. Across all injury acuity, worse MRI injury severity was associated with increased risk of poor outcome, with the largest effects for acute and acute + subacute injuries.