Neonatal Follow-up
NICU Follow Up and Neurodevelopmental 2: Neonatal Growth, Nutrition and the Brain
210 - Does Better Growth Lead to Improved Neurodevelopmental Outcomes in ELBW Infants with Bronchopulmonary Dysplasia?
Friday, April 28, 2023
5:15 PM - 7:15 PM ET
Poster Number: 210
Publication Number: 210.144
Publication Number: 210.144
Fernando A. Munoz, Oregon Health & Science University, Portland, OR, United States; Emily Carter, Oregon Health & Science University School of Medicine, Portland, OR, United States; Erika M.. Edwards, Vermont Oxford Network, Burlington, VT, United States; Maggie Jerome, Oregon Health and Science University, Portland, OR, United States; Jonathan S. Litt, Beth Israel Deaconess Medical Center, Boston, MA, United States

Fernando A. Munoz, MD (he/him/his)
Neonatology Fellow
Oregon Health & Science University
Portland, Oregon, United States
Presenting Author(s)
Background: Infants with bronchopulmonary dysplasia (BPD) are at increased risk for developmental delays compared to peers without BPD. While studies have demonstrated the positive impact of postnatal growth on neurodevelopment in extremely low birth weight (ELBW) infants, no studies have tested whether postnatal growth has a differential effect on developmental outcomes in babies with BPD.
Objective: The objective of this analysis was to examine the relationship between growth rates and 2-year neurodevelopmental outcomes for infants with BPD stratified by disease severity.
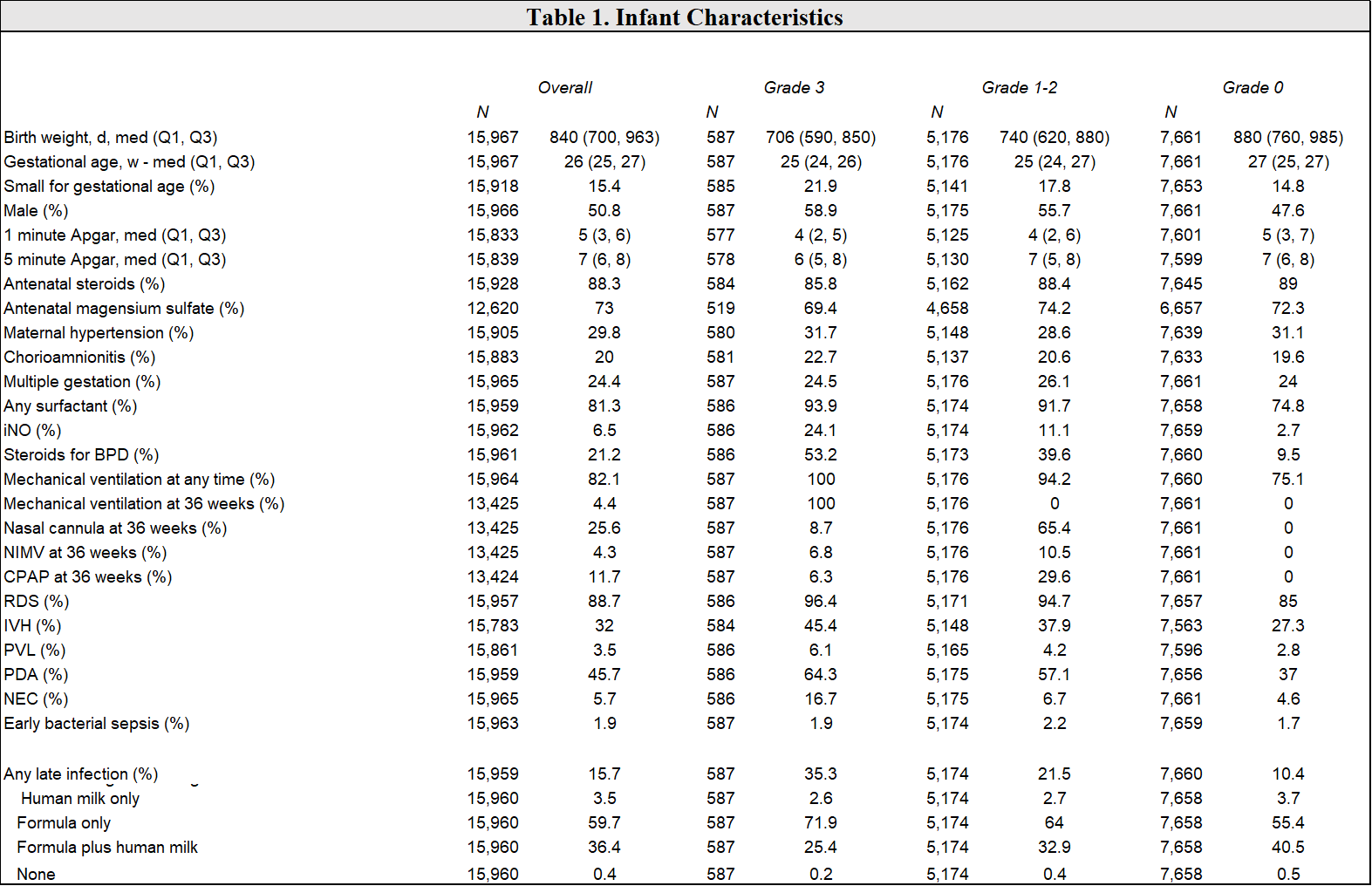
Design/Methods: We performed a secondary analysis of a prospective cohort using data from the Vermont Oxford Network ELBW database. Infants were inborn at participating centers in the U.S and Canada from 2010 to 2019. The primary predictor was BPD, defined as grade 3 (mechanical ventilation at 36 weeks’ postmenstrual age), grade 1-2 (nasal CPAP, ventilation, or cannula at 36 weeks), and grade 0 (no respiratory support at 36 weeks). The primary outcome was neurodevelopmental impairment, defined as any Bayley Scores of Infant Development (BSID) III score < 70 (representing moderate or severe impairment) assessed at 24 months’ corrected age. We used repeated measures logistic regression to test for differential effects of growth defined as weight Z-score at birth, discharge, and follow-up at 24 months corrected gestational age on 2-year neurodevelopmental outcomes by BPD severity. Models were adjusted for gestational age, multiple birth, sex, vaginal delivery, 1-minute Apgar score, and small for gestational age. Infants with congenital anomalies or who were missing growth or BSID data were excluded.
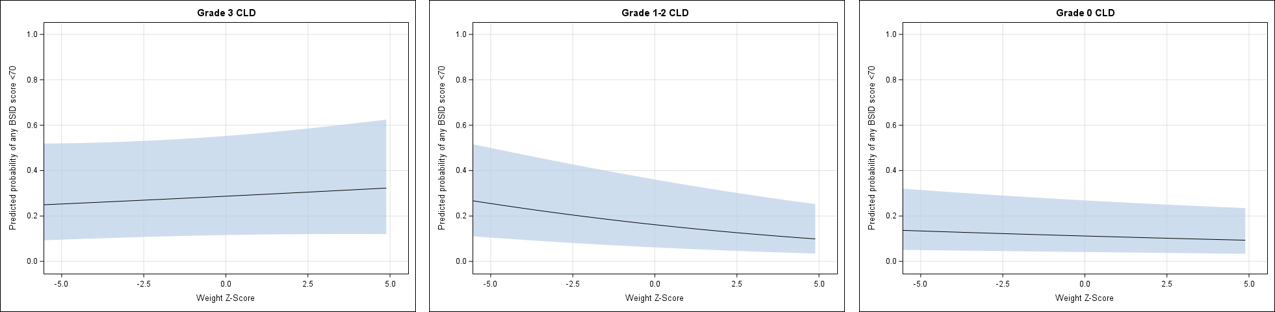
Results: There were 5,509 infants included in the analysis, 3,520 (55.8%) with grade 0 BPD, 2,529 (40.1%) with grade 1-2 BPD, and 259 (4.1%) with grade 3 BPD. Overall, 18.9% of infants had at least one BSID subdomain score < 70. Greater weight gain was significantly associated with a decreased probability of having at least one BSID III score < 70 for grade 1-2 BPD (p< 0.0001), even after adjusting for covariates. There was no significant association between growth and BSID III score < 70 for grade 0 BPD (p< 0.23) or grade 3 BPD (p< 0.73).
Conclusion(s): The association between postnatal growth trajectory and neurodevelopmental outcome differs by BPD severity. Better growth is significantly associated with a decreased risk of moderate to severe neurodevelopmental impairment in infants with grade 1-2 BPD. Further exploration is required to understand the mechanisms by which growth influences neurodevelopment and for only those with moderate lung disease.