Quality Improvement/Patient Safety: Improvement Science Research Methods
QI 1: Improvement Science Research Methods & Evaluation of QI Educational Interventions
675 - Development of a Predictive Model for Cardiac Dysfunction in Multisystem Inflammatory Syndrome in Children: Relevance of Laboratory Biomarkers
Publication Number: 675.151
- BG
Brendan Galdo, Master of Applied Statistics, Master of Arts Psychology
Data Scientist
Nationwide Children's Hospital
Columbus, Ohio, United States
Presenting Author(s)
Background:
Multisystem inflammatory syndrome in children (MIS-C) is a diagnostic challenge. There is an urgent need to identify biomarkers for disease severity prediction.
Objective:
We developed a preliminary predictive algorithm for left ventricular systolic dysfunction (LVSD) or coronary artery anomalies (CAA) using a panel of laboratory parameters from a cohort of MIS-C patients.
Design/Methods:
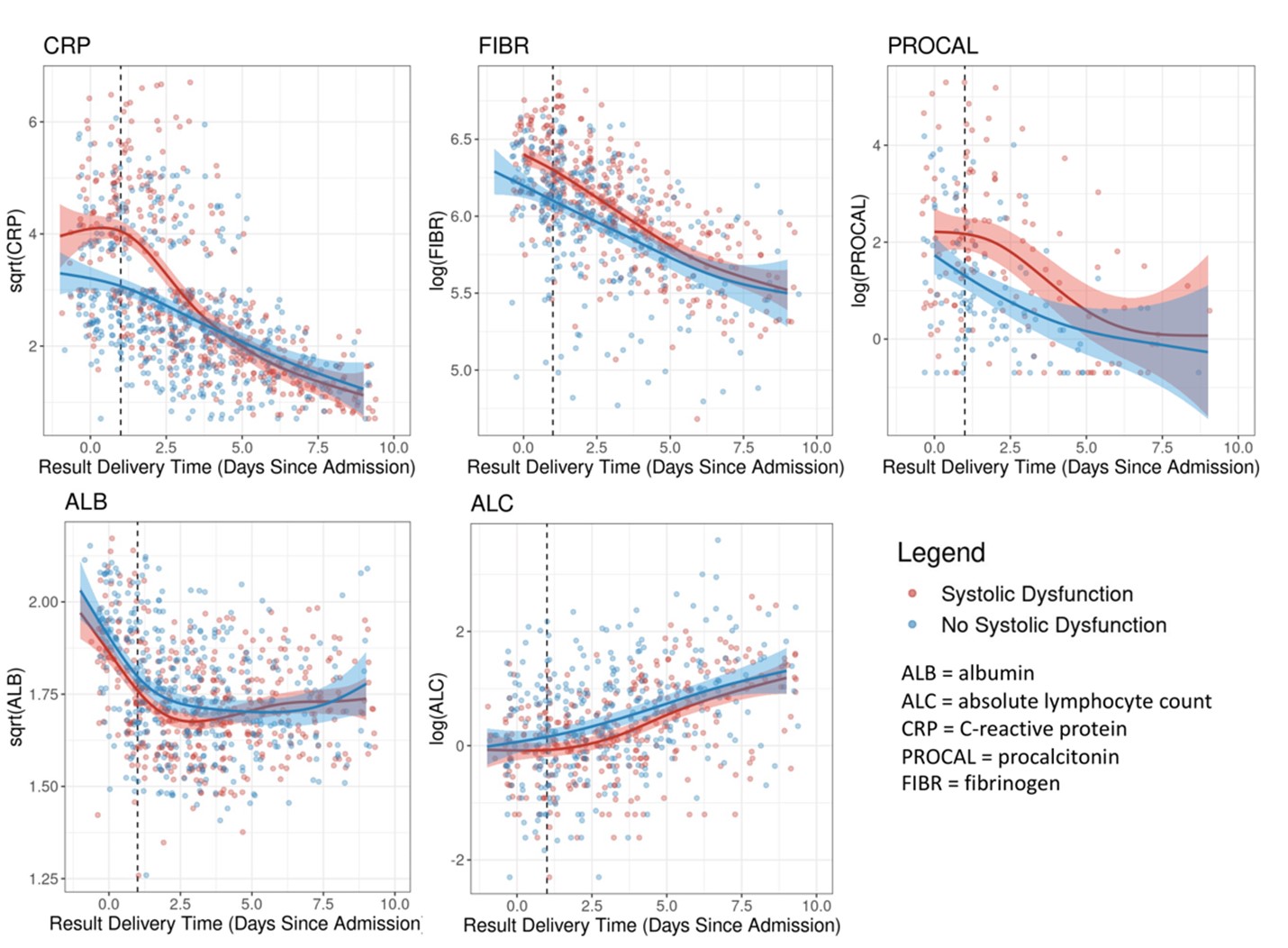
Laboratory and clinical data were collected by retrospective chart review from all patients admitted and treated for MIS-C during a 21-month period at our institution (NCH). Laboratory data collected included absolute lymphocyte count (ALC), albumin (ALB), sedimentation rate (SED), C-reactive protein (CRP), procalcitonin (PROCAL), d-dimer, fibrinogen (FIBR), ferritin (FERR), IL-6, and lymphocyte subsets (TBNK). Candidate biomarkers were selected based on review of published reports for relevant diagnostic and/or predictive tests with a focus on accessibility. The Spearman correlation between the selected variables was assessed. Changes in these measurements across time was determined using spline regression. A regularized logistic regression model was created to predict LVSD and CAA within 24 hours of hospital admission. The performance of this predictive model was assessed using repeated cross-validation.
Results:
160 children were diagnosed and treated for MIS-C. Of these 69 (43%) had LVSD and 27 (17%) had CAA. The time-based analysis of laboratory measurements found univariate differences in mean ALB, ALC, CRP, FIBR, and PROCAL at specific time-points after admission for MIS-C patients with vs. without LVSD. These differences in CRP, FIBR, and PROCAL were notable early on with the mean difference being observed in the first 24 hours of admission. Additionally, we found differences in mean FERR and d-dimer levels for CAA patients. The best LVSD predictive model performed well with a mean cross-validated AUC of 0.78. The predictive biomarkers selected by the LVSD model included: CRP, PROCAL, FIBR, SED, IL6, and absolute NK cell count. The best model for CAA performed poorly with mean cross-validated AUC of 0.57.
Conclusion(s):
We used machine-learning methods to construct mathematical models and identified widely available biomarkers to successfully predict systolic dysfunction in MIS-C patients. Those patients at highest risk of systolic dysfunction had higher peak laboratory values for CRP, PROCAL, and FIBR early on and lower ALB and ALC levels at days 2 and 3 post-admission. Patients with CAA had higher FERR and d-dimer levels, but the effect sizes were small making them less relevant as predictive biomarkers.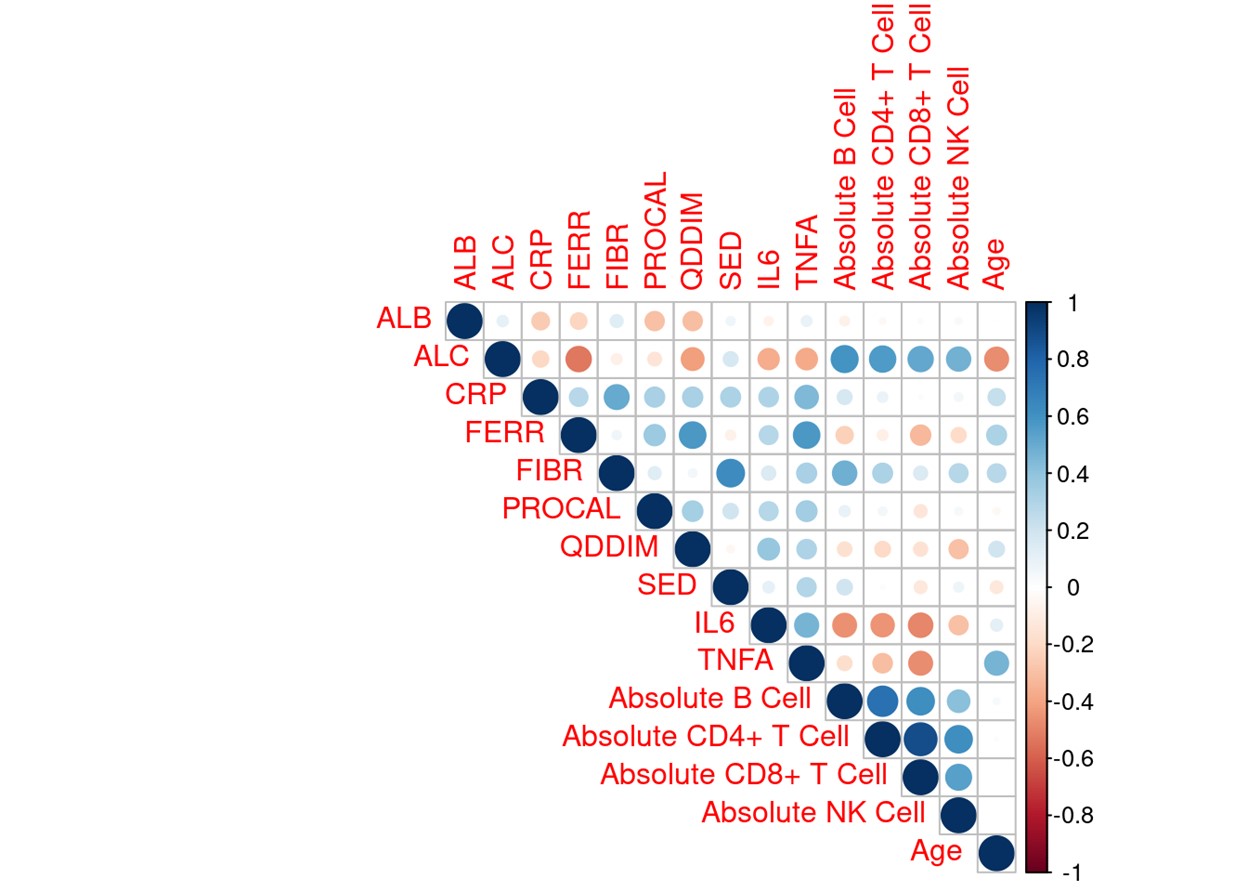
.png)
