General Pediatrics: All Areas
General Pediatrics 1
110 - The Impact of an Antimicrobial and Laboratory Stewardship Clinical Pathway on Outpatient Management of Pediatric Pharyngitis
Publication Number: 110.114
- DN
Diana K. Nguyen, DO (she/her/hers)
Assistant Professor
University of Texas Medical Branch School of Medicine
Galveston, Texas, United States
Presenting Author(s)
Background:
Approximately 7 million pediatric outpatient visits occur each year for pharyngitis. The incidence of Group A Streptococcus (GAS) pharyngitis is uncommon in children < 3 years of age and continues to be a minor contributor to pharyngitis cases amongst older patients, accounting for approximately 20-30% of total cases. Despite clinical guidelines, routine GAS testing in children < 3 years and inappropriate antibiotic administration continues at a high rate. Misdiagnosis of GAS pharyngitis results in unnecessary testing, incorrect antibiotic usage, and increased expenses.
Objective:
Our objective was to improve appropriate testing and treatment of pharyngitis in children < 3 years old in our health system’s ambulatory clinics through clinical pathway dissemination and provider education.
Design/Methods:
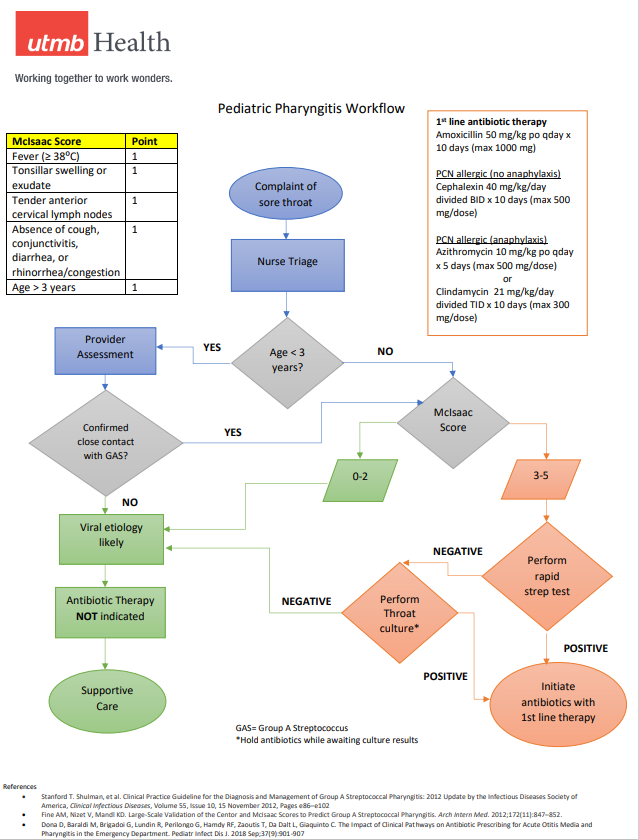
A quality initiative was undertaken by our Lab and Antimicrobial Stewardship Programs from December 2021 through November 2022. An evidence-based pediatric pharyngitis pathway was created using the McIsaac criteria, a validated scoring system as well as recommendations from the 2012 Clinical Practice Guideline from the Infectious Diseases Society of America to guide providers in diagnosis and management of pharyngitis. An informational handout was created for caregivers. The tools were distributed to primary care and urgent care clinics, followed by a live, virtual educational session for providers and nursing staff, emphasizing GAS diagnostic criteria and treatment options. Primary outcomes included reduction of GAS rapid tests performed on children < 3 years of age and reduction of antibiotic prescriptions for pharyngitis when there was either a negative GAS test or no test performed by 10% within 1 year of implementing the pharyngitis clinical pathway. Outcomes were tracked monthly and compared to the baseline period of December 2020 through November 2021.
Results:
There were 1904 visits for pharyngitis in children < 3 years old during the implementation period. The percentage of GAS tests performed decreased from a baseline of 37.6% to 33.2% (p = 0.952). The percentage of visits with an antibiotic prescription for pharyngitis when the GAS test was negative or when no test was done decreased from 69.9% to 36.0% (p < 0.00001). Results were analyzed using a two-tailed Z test.
Conclusion(s):
Implementation of a pharyngitis clinical pathway and provider education can reduce unnecessary testing and antibiotic prescriptions, though the latter had more impact. This method can be used for other common pediatric infections to expand laboratory and antimicrobial stewardship in the outpatient setting. 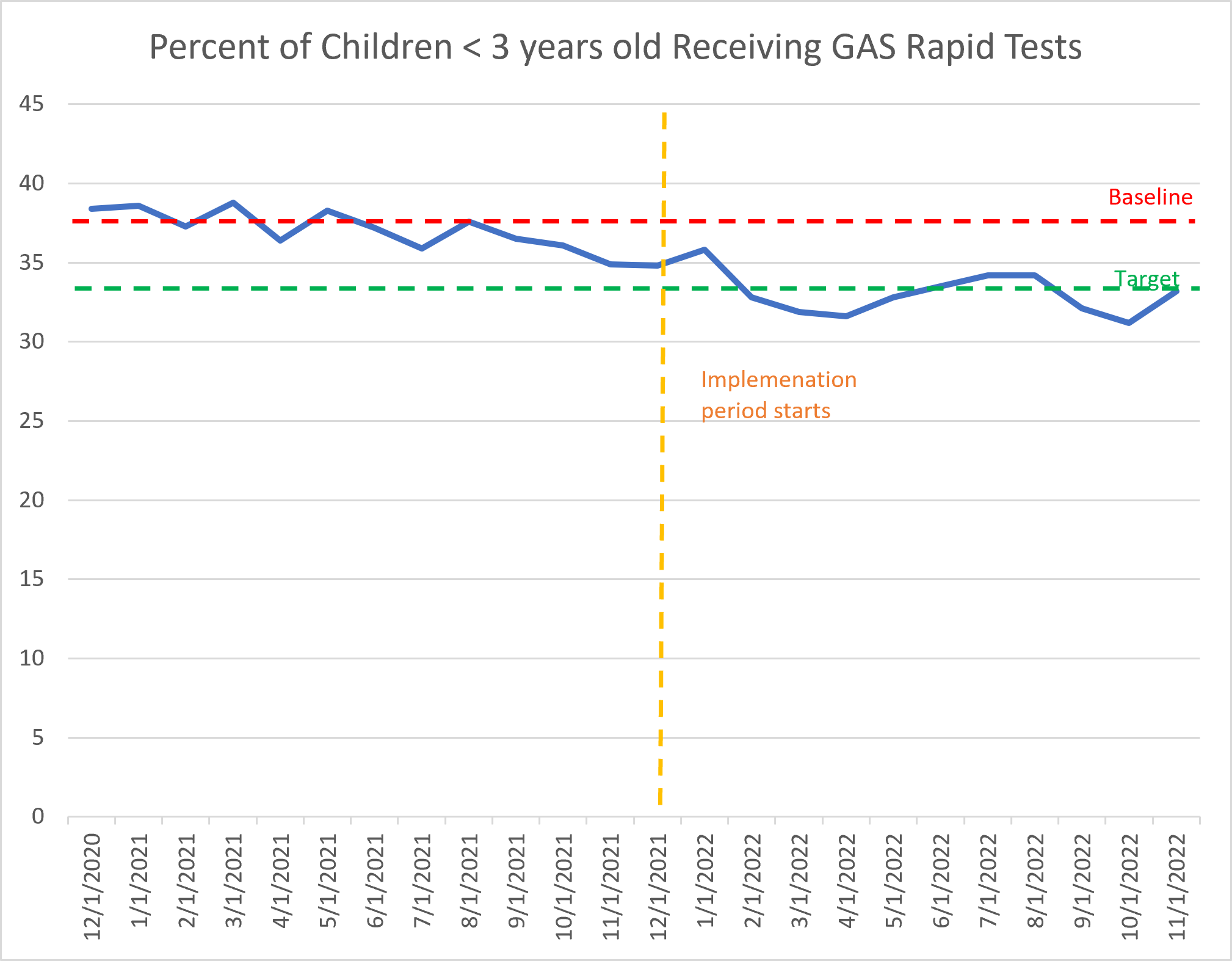
.png)