Neonatal Neurology: Clinical Research
Neonatal Neurology 3: Clinical 3
179 - How well does neonatal neuroimaging correlate with neurodevelopmental outcomes in infants with hypoxic-ischemic encephalopathy (HIE)?
Publication Number: 179.137
- YW
Yvonne Wu, MD MPH (she/her/hers)
Professor of Neurology and Pediatrics
UCSF
San Francisco, California, United States
Presenting Author(s)
Background:
Neonatal brain MRI and MRS findings are important biomarkers of long-term outcome in infants with HIE. However, the prognostic value of neonatal neuroimaging findings for predicting degree of neurodevelopmental impairment (NDI) after HIE remains unclear.
Objective:
To determine how well neonatal neuroimaging predicts HIE outcomes within a large multicenter clinical trial.
Design/Methods:
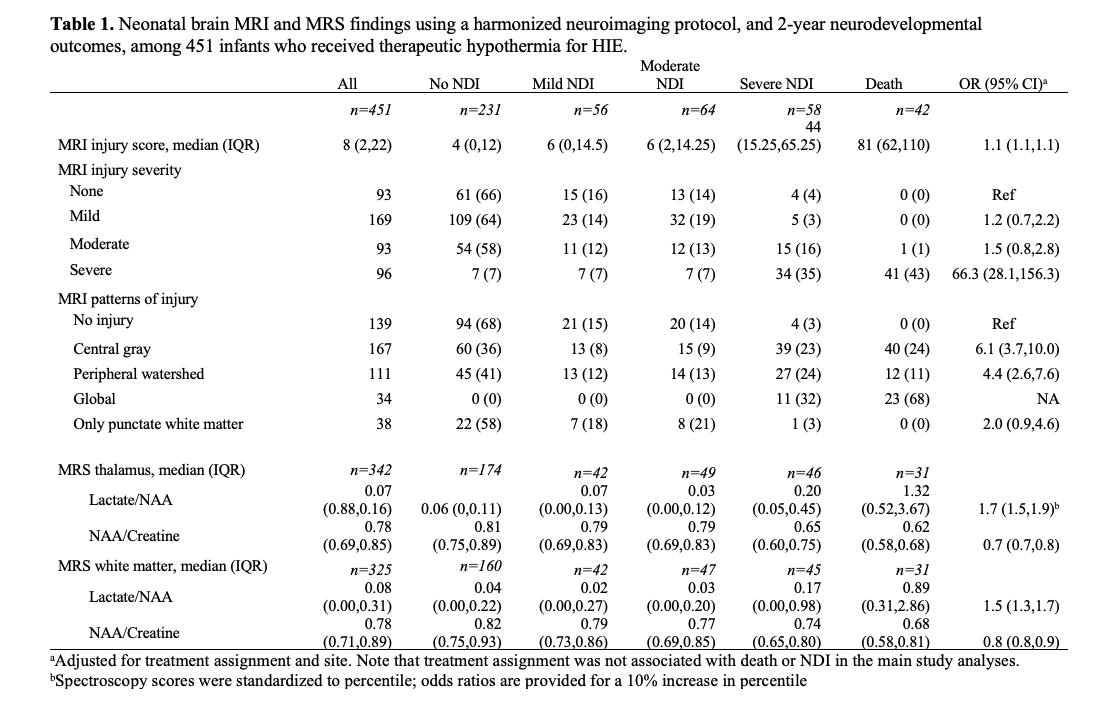
Infants with moderate or severe HIE enrolled in a randomized controlled trial (HEAL) underwent neonatal MRI/MR spectroscopy (MRS) using a harmonized protocol at 4-6 days of age. Severity of MRI brain injury was measured with a validated scoring system. Using proportional odds regression, we calculated adjusted odds ratios (aOR) for the associations between MRI and MRS measures of injury, and the 2-year primary ordinal outcome measure: no NDI, mild NDI, moderate NDI, severe NDI, or death.
Results:
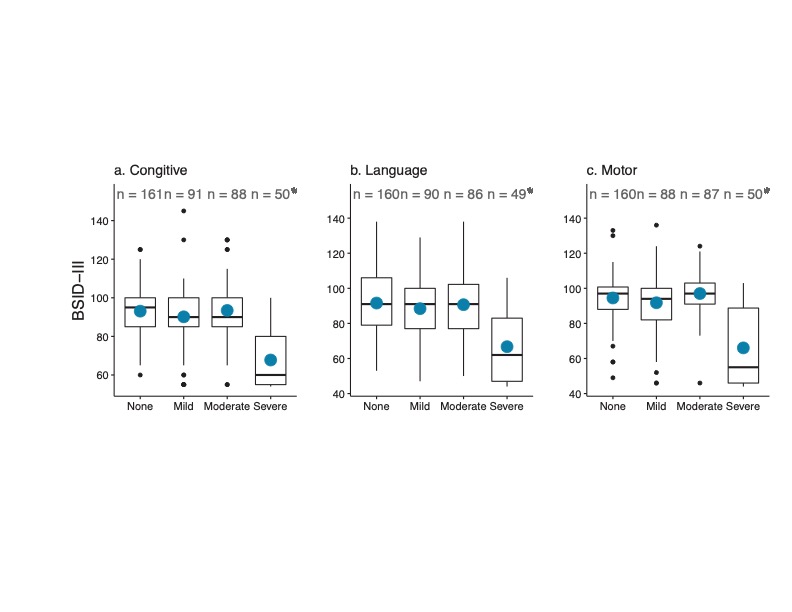
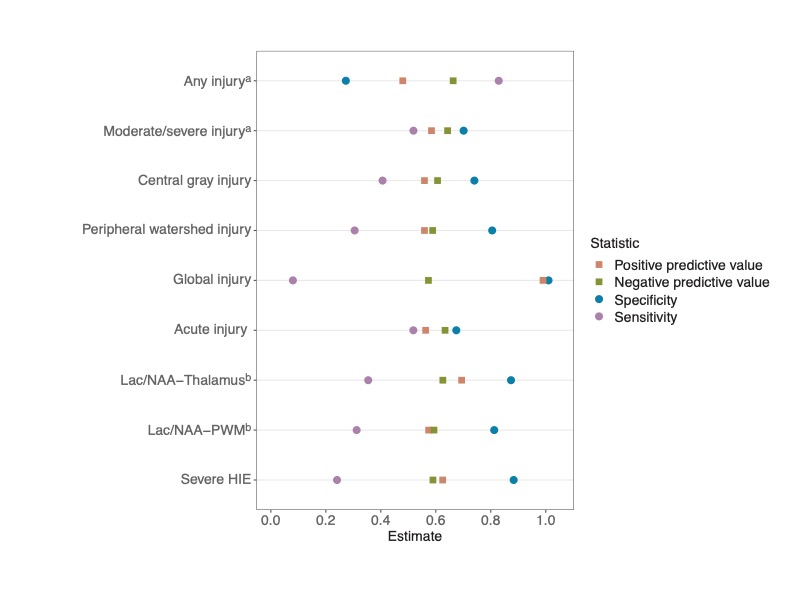
Of 451 infants with MRI/MRS at median age 5 days (IQR 4.5-5.8), outcomes were no (51%), mild (12%), moderate (14%), severe NDI (13%); or death (9%). All 34 infants with global injury on MRI either died or had severe NDI. Severe brain injury (aOR 39.6, 95% CI 16.4,95.6), MRS lactate/n-acetylaspartate (NAA) ratio (aOR 1.6, 95% CI 1.4,1.8) and MRI injury score (aOR 1.06, 95% CI 1.05,1.07) were associated with worse primary outcome (Table 1). Of 93 infants with no injury on MRI, 66% had no NDI; the remaining had mild (16%), moderate (14%), or severe (4%) NDI. Among survivors, infants with a mild or moderate degree of MRI brain injury had similar BSID-III cognitive, language and motor scores as infants with no injury (Figure 1). Infants with a lactate/NAA ratio in the second or third quartiles also had similar BSID-III scores as infants with ratios in the lowest quartile. The positive predictive values of MRI and MRS features for predicting death or NDI at age 2 years are shown in Figure 2. Other than MRI global injury which perfectly predicted poor outcome, the positive predictive values of other neuroimaging features ranged from 0.48 to 0.69 and their negative predictive values ranged from 0.57 to 0.66. The clinical determination of severe HIE based on Sarnat examination had a positive predictive value of 0.63 and negative predictive value of 0.59 (Figure 2).
Conclusion(s):
In the absence of global or severe injury, brain MRI on its own does not accurately discriminate degree of NDI. Given this prognostic uncertainty among infants with less severe degrees of brain injury, families should be counseled regarding a range of possible neurodevelopmental outcomes.