Emergency Medicine: All Areas
Emergency Medicine 1
20 - Is SIRS a Predictor of Bacteremia in Patients with Central Lines when Presenting to a Pediatric Emergency Department?
Publication Number: 20.11
.jpg)
Maria E. Arrate, Doctor of Osteopathic Medicine
Resident
Nicklaus Children’s Hospital
Miami , Florida, United States
Presenting Author(s)
Background:
Bacteremia, while uncommon in pediatric patients, is more prevalent in those with central lines and is associated with an increased risk of mortality. Risk of bacteremia increases when a central line is present, with an incidence of up to 10% when compared to 0.4% in those without central lines. The utility of the Systemic Inflammatory Response Syndrome (SIRS) criteria as a predictor of bacteremia in patients with a central line has yet to be studied.
Objective:
1. To determine if SIRS criteria can be used to predict bacteremia in pediatric patients with central lines presenting with fever to the emergency department (ED). 2. Calculate the diagnostic characteristics of SIRS for identifying bacteremia.
Design/Methods:
Single institution retrospective cohort study of pediatric patients from 0-21 years old who presented to the ED with central lines and had a blood culture drawn in the ED between April 2012 to May 2021.Patients were characterized with SIRS if any one of serval combinations of SIRS criteria were met, using the most extreme age specific vital signs during their visit as classification. Multivariable logistic regression was used to measure the association between SIRS and bacteremia while adjusting for potential confounders. The diagnostic characteristics of SIRS criteria for the identification of bacteremia according to the number of criteria met were calculated.
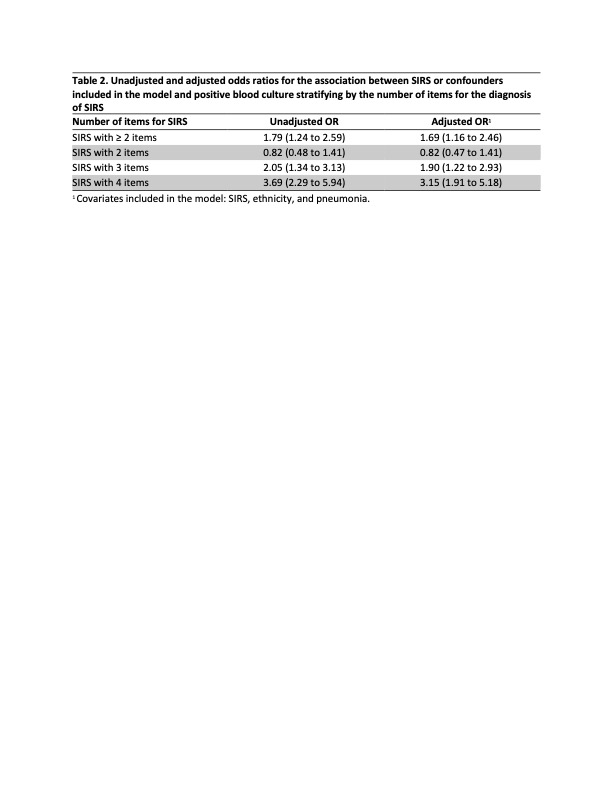
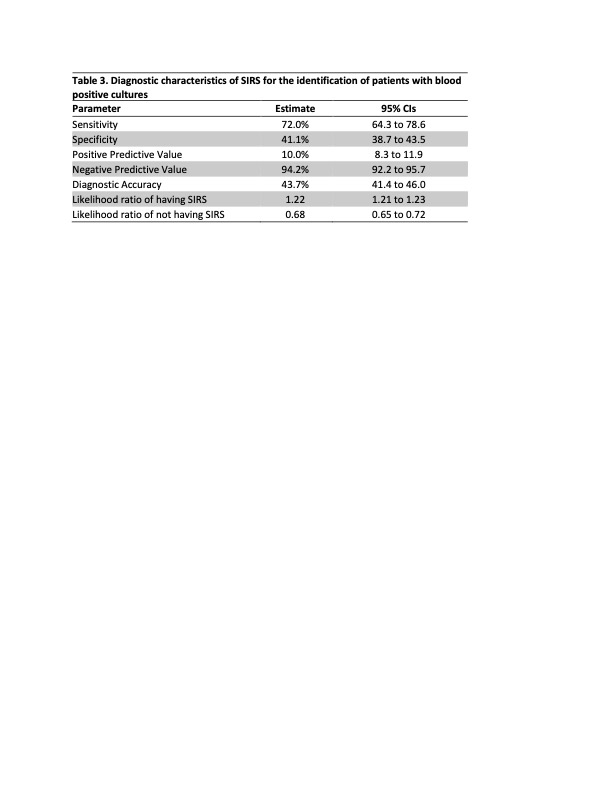
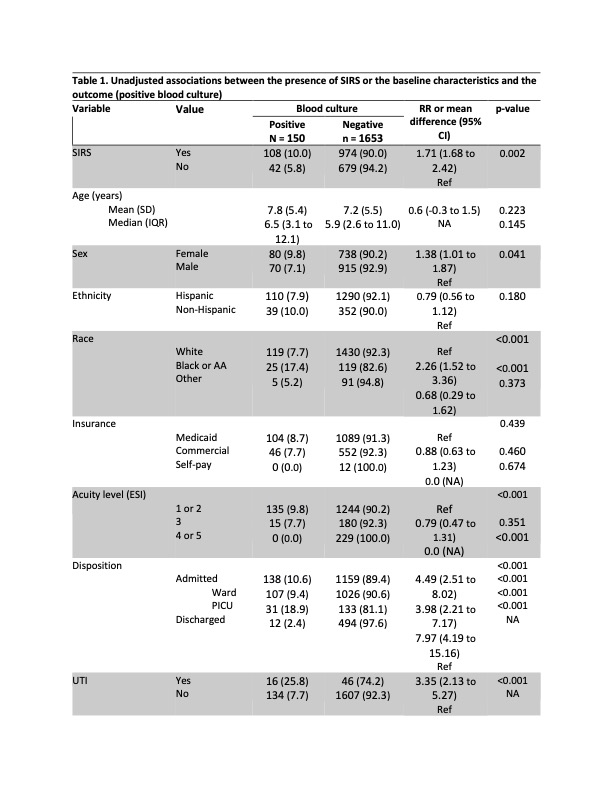
Results: 1,803 total patients with central lines had blood cultures drawn in the ED with 1,082 (60%) of those meeting SIRS criteria (Table 1). Overall, 150 patients (8.3%) had bacteremia. Of those who met SIRS criteria with bacteremia, 53% were female and 47% were male, with a mean age of 7.8 years. The adjusted odds ratio (aOR) of bacteremia in patients with SIRS was 1.69 (95% CI 1.16 to 2.46) (Table 2). The odds of bacteremia increased with the number of SIRS criteria met. 2 criteria: aOR 0.82 (0.47 to 1.41); 3 criteria: aOR 1.90 (1.22 to 2.93); and 4 criteria: aOR 3.15 (1.91 to 5.18) (Table 2). Overall, the sensitivity of SIRS for identifying bacteremia was 72%, specificity 41.1%, positive predictive value 10%, negative predictive value 94.2% (Table 3). Sensitivity and specificity increased as the number of SIRS criteria increased.
Conclusion(s):
SIRS is a limited predictor of bacteremia in pediatric patients with central lines (aOR 1.69, 72% sensitivity and 41% specificity). Having multiple SIRS criteria increased the odds of having bacteremia.