Back
Background: Several approaches have been developed to predict the risk of invasive bacterial infection (IBI) in febrile oncology patients. Risk factors may vary in patients with hematologic malignancies and solid tumors. Additionally, it would be useful to identify predictors specifically for eventually developing a sepsis.
Objective: To identify clinical and analytical risk factors of IBI and specifically for developing a sepsis in febrile oncology patients attended in the pediatric emergency department (PED) by type of cancer.
Design/Methods: Prospective observational study of oncology patients receiving chemotherapy who attended the PED of a tertiary teaching hospital between 2016 and 2021. We defined IBI as the growth of:
< !- a bacterial pathogen in blood, cerebrospinal fluid or any other sterile fluid
- - - a bacterium commonly considered contaminant in two blood cultures obtained simultaneously from a peripheral vein and a central venous catheter (CVC), usually port-a-cath, or in two different samples obtained from a CVC: catheter-related bloodstream infection (CRBSI).
We performed two separate multivariate analysis in hematologic malignancies and solid tumors, including the following variables: sex, age, general appearance, fever degree, absolute neutrophil count (ANC), monocyte count and C-reactive protein and procalcitonin values. In the analysis of patients with hematologic malignancies we also included the type of malignancy (high-risk: acute lymphoblastic leukemia or non-Hodgkin lymphoma in induction/reinduction/consolidation phase or relapsed and acute myeloid leukemia in any phase)
Results: We included 394 episodes (256 hematologic malignancies and 138 solid tumors) in 145 children. Median ANC was 680/mcL (IQR 100-3220) and median evolution time of fever was 2 hours (IQR 1-3). We diagnosed 57 IBIs (14.5%): 31 CRBSI, 16 sepsis, 9 bacteremia and 1 bacterial meningitis. Six additional patients had sepsis with no microbiological confirmation, for a total of 22 cases of sepsis (5.5%).
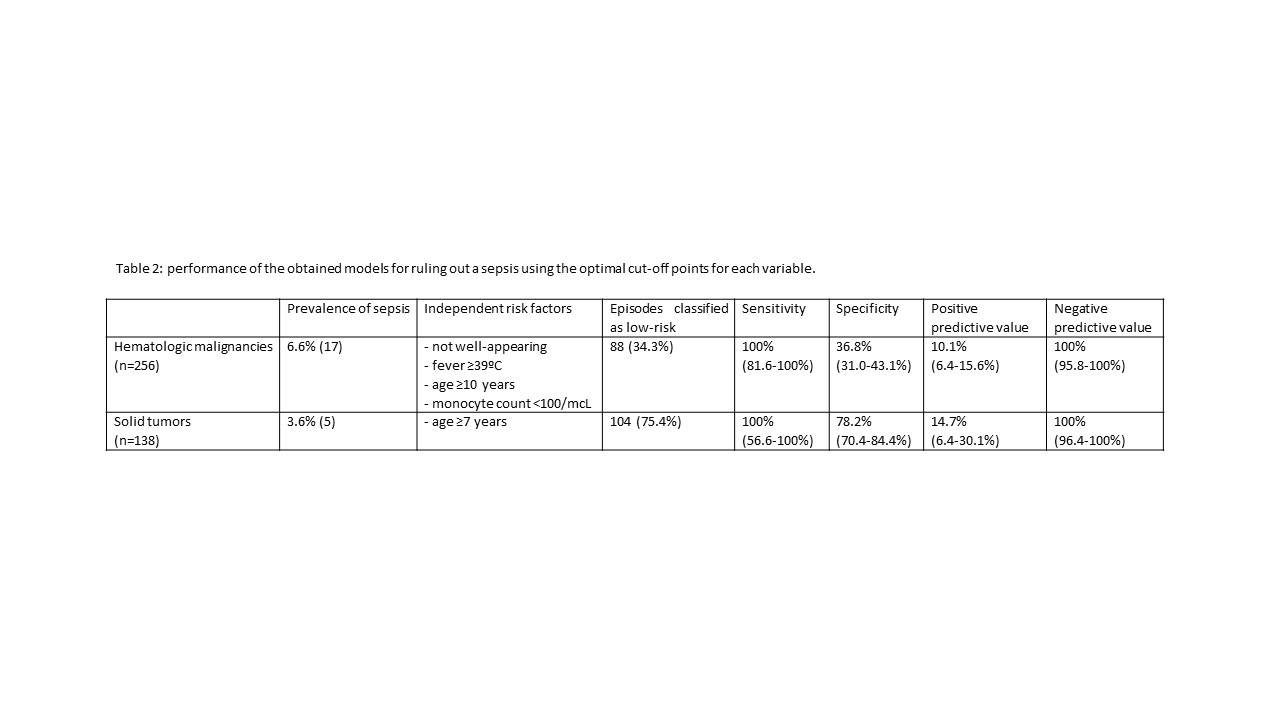
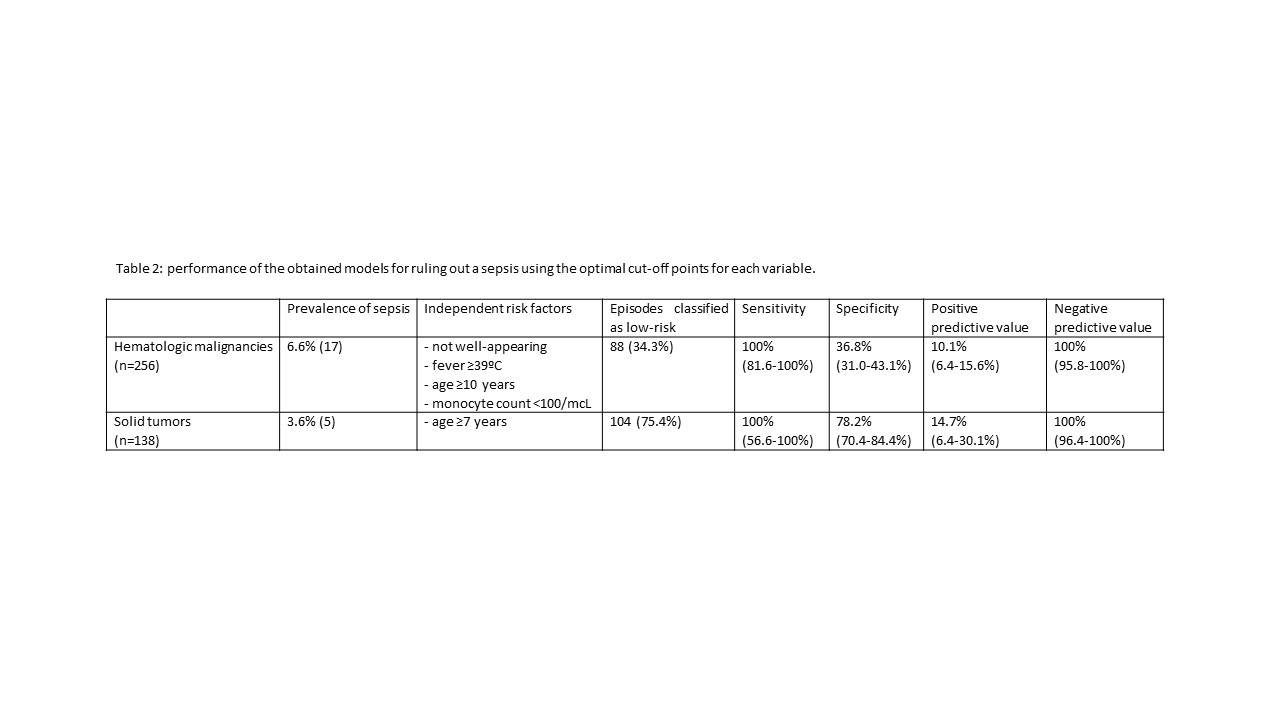
Table 1 shows the independent risk factors identified by type of cancer. Table 2 shows the performance of the obtained models for ruling out a sepsis using the optimal cut-off points for each variable.
Conclusion(s): We identified clinical and analytical risk factors for IBI and specifically for developing a sepsis that can guide initial clinical decision-making in febrile patients with hematologic malignancies. ANC on arrival was not an independent risk factor. Multicenter studies are necessary to confirm these results and to obtain more useful findings in patients with solid tumors.
.jpg)
Emergency Medicine: All Areas
Emergency Medicine 1
19 - Risk factors for invasive bacterial infection and specifically for sepsis in febrile oncology patients according to the type of cancer
Friday, April 28, 2023
5:15 PM – 7:15 PM ET
Poster Number: 19
Publication Number: 19.11
Publication Number: 19.11
Borja Gomez, Cruces University Hospital, Barakaldo, Pais Vasco, Spain; Oriol Quintana, Hospital Universitario Cruces, Bilbao, Pais Vasco, Spain; Fernando Almarza, Hospital Universitario Cruces, Bilbao, Pais Vasco, Spain; Mirian Moreno, Hospital universitario de Cruces, Bilbao, Pais Vasco, Spain; Ricardo Lopez Almaraz, Hospital Universitario Cruces; IIS Biocruces Bizkaia, Baracaldo, Pais Vasco, Spain; Santiago Mintegi, Hospital Universitario Cruces, Bilbao, Pais Vasco, Spain

Borja Gomez, MD, PhD (he/him/his)
Pediatric Emergency Physician
Cruces University Hospital
Barakaldo, Pais Vasco, Spain
Presenting Author(s)
Background: Several approaches have been developed to predict the risk of invasive bacterial infection (IBI) in febrile oncology patients. Risk factors may vary in patients with hematologic malignancies and solid tumors. Additionally, it would be useful to identify predictors specifically for eventually developing a sepsis.
Objective: To identify clinical and analytical risk factors of IBI and specifically for developing a sepsis in febrile oncology patients attended in the pediatric emergency department (PED) by type of cancer.
Design/Methods: Prospective observational study of oncology patients receiving chemotherapy who attended the PED of a tertiary teaching hospital between 2016 and 2021. We defined IBI as the growth of:
< !- a bacterial pathogen in blood, cerebrospinal fluid or any other sterile fluid
- - - a bacterium commonly considered contaminant in two blood cultures obtained simultaneously from a peripheral vein and a central venous catheter (CVC), usually port-a-cath, or in two different samples obtained from a CVC: catheter-related bloodstream infection (CRBSI).
We performed two separate multivariate analysis in hematologic malignancies and solid tumors, including the following variables: sex, age, general appearance, fever degree, absolute neutrophil count (ANC), monocyte count and C-reactive protein and procalcitonin values. In the analysis of patients with hematologic malignancies we also included the type of malignancy (high-risk: acute lymphoblastic leukemia or non-Hodgkin lymphoma in induction/reinduction/consolidation phase or relapsed and acute myeloid leukemia in any phase)
Results: We included 394 episodes (256 hematologic malignancies and 138 solid tumors) in 145 children. Median ANC was 680/mcL (IQR 100-3220) and median evolution time of fever was 2 hours (IQR 1-3). We diagnosed 57 IBIs (14.5%): 31 CRBSI, 16 sepsis, 9 bacteremia and 1 bacterial meningitis. Six additional patients had sepsis with no microbiological confirmation, for a total of 22 cases of sepsis (5.5%).
Table 1 shows the independent risk factors identified by type of cancer. Table 2 shows the performance of the obtained models for ruling out a sepsis using the optimal cut-off points for each variable.
Conclusion(s): We identified clinical and analytical risk factors for IBI and specifically for developing a sepsis that can guide initial clinical decision-making in febrile patients with hematologic malignancies. ANC on arrival was not an independent risk factor. Multicenter studies are necessary to confirm these results and to obtain more useful findings in patients with solid tumors.
.jpg)