Neonatal Quality Improvement
Neonatal Quality Improvement 2
659 - Revamping a Multidisciplinary Team with Phased Targeted Approach to Reduce Unplanned Extubation in the NICU
Friday, April 28, 2023
5:15 PM - 7:15 PM ET
Poster Number: 659
Publication Number: 659.139
Publication Number: 659.139
Parvathy Krishnan, Maria Fareri Children's Hospital at Westchester Medical Center, white plains, NY, United States; Nilima Jawale, State University of New York Upstate Medical University, Binghamton, NY, United States; Susan R.. Malfa, Maria Fareri Children's Hospital, Pleasantville, NY, United States; Kathleen McCarthy, Maria Fareri Children's Hospital at Westchester Medical Center, Nanuet, NY, United States; Diana D'Agrosa, Maria Fareri Children's Hospital at Westchester Medical Center, Valhalla, NY, United States; Jason Muglio, Maria Fareri Children's Hospital at Westchester Medical Center, Brewster, NY, United States; Adam Sodikoff, Westchester Medical Center, Richmond Hill, NY, United States; Colby Riehman, Maria Fareri Children's Hospital at Westchester Medical Center, Valhalla, NY, United States; Alexandra Pickard, Westchester Medical Center, Eastchester, NY, United States; Lisa M.. Strickrodt, Maria Fareri Children's Hospital at Westchester Medical Center, Newtown, CT, United States; Lance A. Parton, Maria Fareri Children's Hospital at Westchester Medical Center, Valhalla, NY, United States; Meenakshi Singh, Maria Fareri Children's Hospital at Westchester Medical Center, Valhalla, NY, United States

Parvathy Krishnan, MBBS (she/her/hers)
Fellow
Maria Fareri Children's Hospital at Westchester Medical Center
white plains, New York, United States
Presenting Author(s)
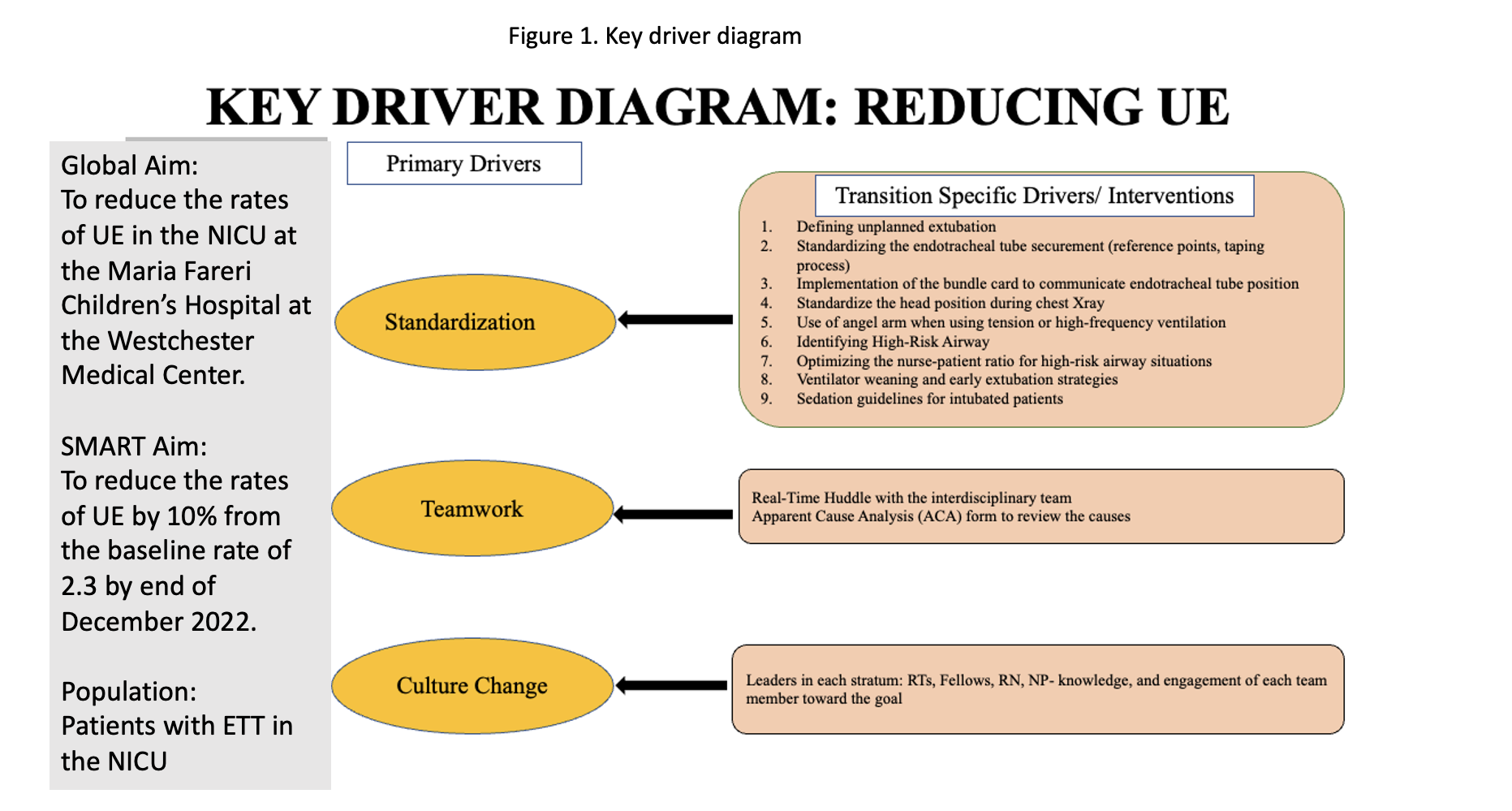
Background: Unplanned Extubation (UE) is an important patient safety issue in the NICU. UE is associated with short and long-term cardiorespiratory and neurological complications. A comprehensive and sustained model for reducing UE is necessary.
Objective:
SMART
Aim: To decrease the rate of unplanned extubation by 10% from the historical mean (January to December 2021) by the end of December 2022.
Design/Methods:
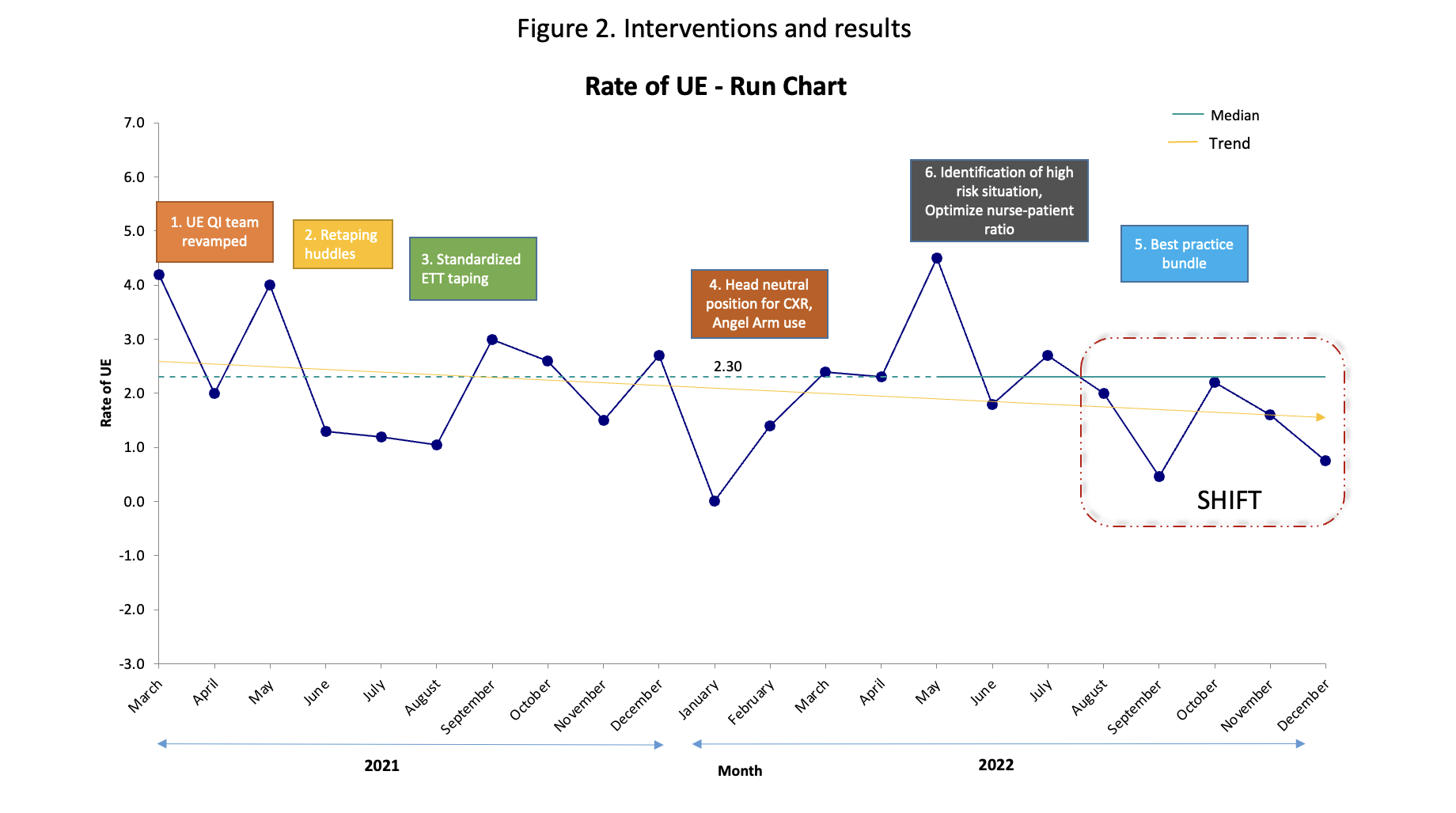
This was a quality improvement (QI) project involving the intubated infants in the NICU at the Maria Fareri Children’s Hospital at the Westchester Medical Center launched in the first quarter of 2021. An interdisciplinary QI team was formed. The definition of UE was standardized. All UE were identified using a data collection tool (ACA- apparent cause analysis form). The clinical team, including the nurse, medical provider, and respiratory therapist, completed the ACA form in real-time. ACA form was used to identify the causes related to UE and key areas for improvement.(Fig 1) Interventions were implemented in a step-by-step fashion and reviewed monthly using the Plan-Do-Study-Act (PDSA) model.
Interventions included retaping huddles, standardizing the ETT holding and taping, ensuring midline head position during chest X-ray, using an angel arm to stabilize ETT, identifying high-risk patients, providing optimal nurse/patient ratio and 2 providers for repositioning. An educational tool was created and placed bedside of the intubated patients reminding the components of the best practice bundle.
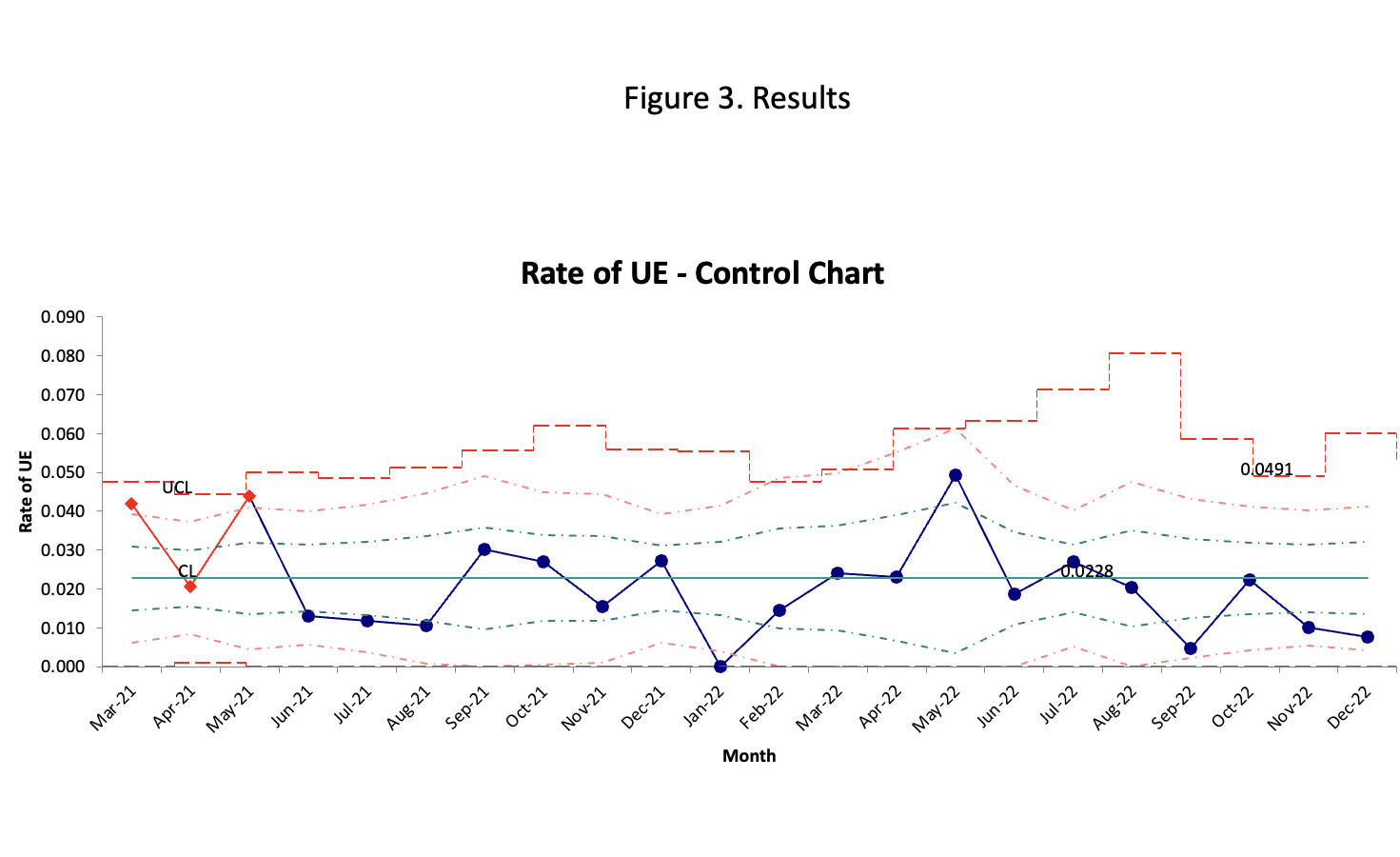
The causes of UE were constantly analyzed using Pareto charts. Shewhart chart and run chart were used to measure the monthly trend and special cause variation.
Results:
Baseline data:
From March 2021 to January 2023, the ventilator days ranged from 61 to 300 days per month. Our average baseline UE rate was 2.3/100 ventilator days. Retaping, bedside procedures, and repositioning accounted for over 50% of the UE events. 86% of the events required reintubation.
Results:
Step-by-step interventions and results as in Fig 2.
The rate of UE was reduced by 20% by the end of December 2022. Over the last 5 months from August 2022- December 2022, we achieved rates of UE consistently below the median of 2.3 UE/ 100 ventilator days. (Fig 3)
Conclusion(s):
Our UE rates continue to trend below the median. If this trend continues for another month, then it is a “shift” and special cause variation suggesting a significant change in the system. Significant UE rate reduction was achieved by continuously evaluating high-risk factors and ensuring the implementation of best practices in a sequential manner.