Emergency Medicine: All Areas
Emergency Medicine 4
63 - Characteristics and Outcomes of Patients Boarding in the Pediatric Emergency Department in the Post-COVID Era
Publication Number: 63.112

Brandon Kappy, MD, MPP
Fellow in Pediatric Emergency Medicine
Children's National Health System
Washington, District of Columbia, United States
Presenting Author(s)
Background:
Emergency Departments (ED) have been under strain since the spread of COVID-19 variants and the reemergence of respiratory viral illnesses converged with staffing shortages and decreased bed capacity. Boarding admitted patients in the ED has been shown to cause throughput delays in adults, though few studies have examined pediatric boarding. Adult studies have shown associations between boarding and inpatient length-of-stay (LOS) and mortality.
Objective:
To characterize the boarding times and clinical attributes of admitted patients boarding in the pediatric ED between 2018–2022 and assess associations with hospital LOS by patient diagnosis.
Design/Methods:
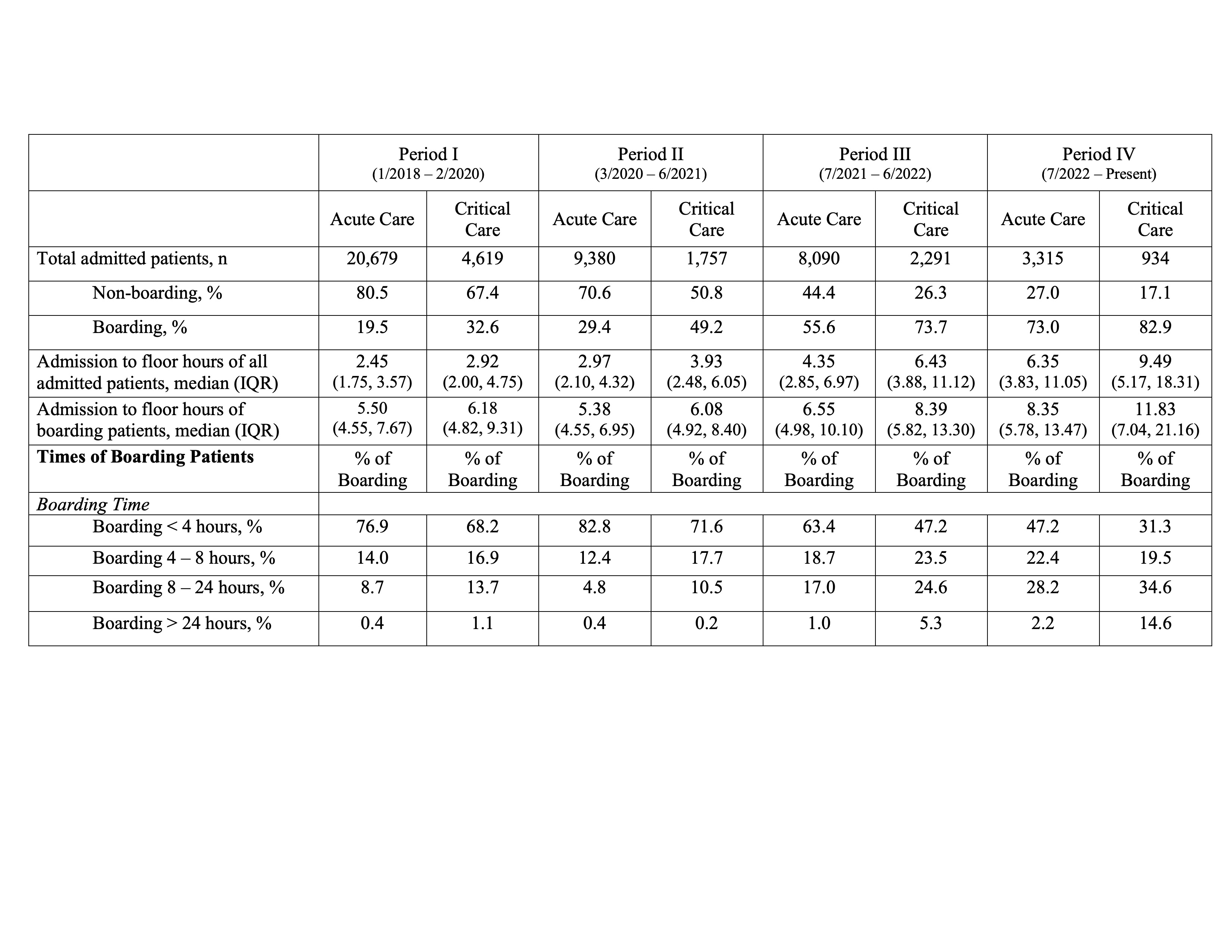
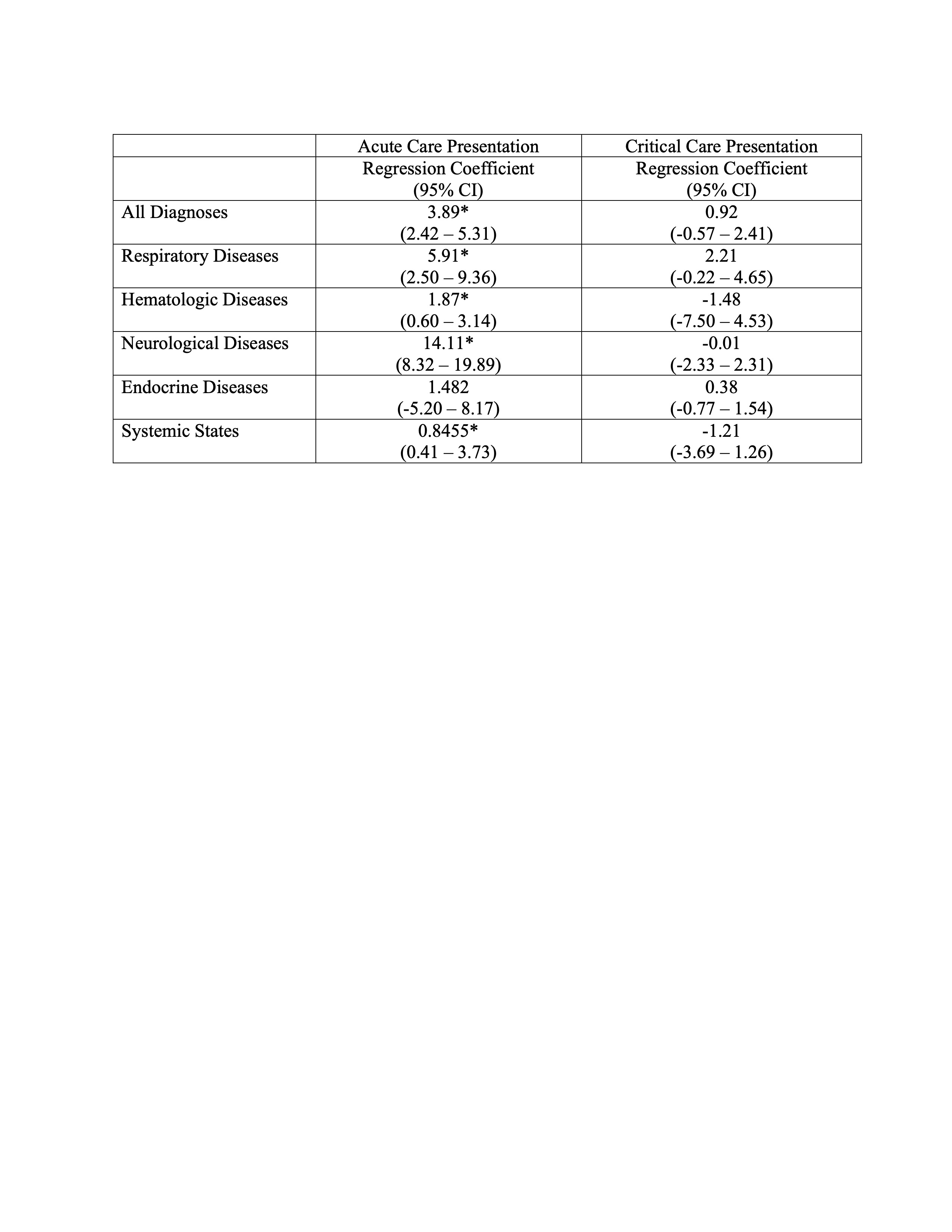
We performed a retrospective analysis of all patients with non-psychiatric complaints who presented to a pediatric ED between 2018—2022, broken into four periods: pre-pandemic (Period I: 1/2018–2/2020), the beginning of the COVID-19 pandemic (II: 3/2020–6/2021), the emergence of COVID-19 variants (III: 7/2021–6/2022), and the reemergence of non-COVID respiratory viruses (IV: 7/2022–12/2022). We defined boarding as beginning 4 hr after a patient was admitted to the hospital from the ED and categorized boarding times as short (< 4), intermediate (4–8), prolonged (8–24), or multi-day ( >24). Patients were classified as critical care or acute care based on their initial bed request. We compared descriptive statistics for boarding times across periods, according to admitting service. We used linear regression to model the relationship between boarding time and hospital LOS for 7/2021–12/2022, based on Pediatric Emergency Care Applied Research Network diagnosis groupings of ICD-10 codes.
Results:
Boarding rates increased for Period III (acute: 55.6%, critical: 73.7%) and IV (73.0%, 82.9%), compared to Period I (19.5%, 32.6%). During Period IV, a higher proportion of admitted patients boarded for 8–24 hr (acute: 28.2%, critical: 34.6%) compared to Period I (8.7%, 13.7%). Between 7/2021—12/2022, each additional hour of acute care boarding was associated with an increase of 3.89 hr (95%CI: 2.42, 5.31) in hospital LOS; increases in hospital LOS were more pronounced for patients with respiratory (5.91 CI: 2.50, 9.36) and neurological diseases (14.11 CI: 8.32, 19.89). Critical care boarding was not significantly associated with hospital LOS.
Conclusion(s):
Since 7/2021, there has been an unprecedented increase in boarding rates and time for patients admitted to acute and critical care services. Length of time boarding in the ED was associated with large increases in hospital LOS for most acute care admissions, but not critical care admissions.