Neonatal Follow-up
NICU Follow Up and Neurodevelopment 1: Developmental and Sensory Disorders
192 - Characterization of Clinical MRI Findings in Moderately-Late Preterm Infants Diagnosed with Cerebral Palsy: A Single Center Retrospective Study
Publication Number: 192.142
- DM
Divakar S. Mithal, MD, PhD (he/him/his)
Clinical instructor
Ann & Robert H. Lurie Children's Hospital of Chicago/Northwestern University Feinberg School of Medicine
Chicago, Illinois, United States
Presenting Author(s)
Background:
Cerebral palsy (CP) is a clinical syndrome characterized by impaired movement and posture, and is the most common movement disorder among children. The myriad causes of CP range from genetics to brain injury which can cause confusion for patients and families. Still, 75% of patients with CP value knowing their etiology and would prefer to carry both a CP and etiological diagnosis. In term infants, evidence of brain injury on MRI is identified as the leading cause of CP; however, premature birth under 36 weeks gestational age (WGA) does not have the same imaging-phenotype association. Furthermore, premature children with CP have higher rates of possible neurologic complications such as tracheostomy, gastrostomy or epilepsy. Characterization of the types and distributions of premature brain MRI findings may help reduce diagnostic and prognostic confusion regarding disease severity.
Objective: The central hypothesis in the project is that moderately premature infants, with defined, acquired brain injuries have a more severe clinical presentation than those with non-specific MRI findings. The study tests the hypothesis by categorizing the spectrum of moderately pre-term CP patient MRI findings and comparing clinical parameters.
Design/Methods:
A retrospective cohort study of infants born at Lurie Children’s Hospital between 2007 and 2020 identified all children with a CP ICD code. CP patients born between 32 and 34 WGA were selected as a moderately pre-mature group. Clinical data, including MRI imaging was extracted from the electronic medical record. MRI were grouped into five categories based on existing literature for moderately premature brain imaging (Table 1). Two independent, board-certified pediatric neuroradiologists reviewed the imaging patterns to gain consensus on the categorization.
Results:
5014 total patients with CP were identified of whom 104 were born between 32 and 34 WGA, and 64 had MRI imaging available for review. 54% had a defined causal injury associated with CP (Figure 1). Importantly, patients with nonspecific findings that were unlikely to be causative of the clinical picture, had statistically similar rates of a gastrostomy, tracheostomy or epilepsy as patients with more severe imaging patterns (Figure 2).
Conclusion(s):
Children with CP who are born moderately preterm frequently have nonspecific MRI findings. Imaging findings do not correlate with overall disease severity, indicating that for this population, the severity of brain injury on MRI is a poor predictor of neurologic outcome. The risk factors conferring poor neurologic outcome require further investigation.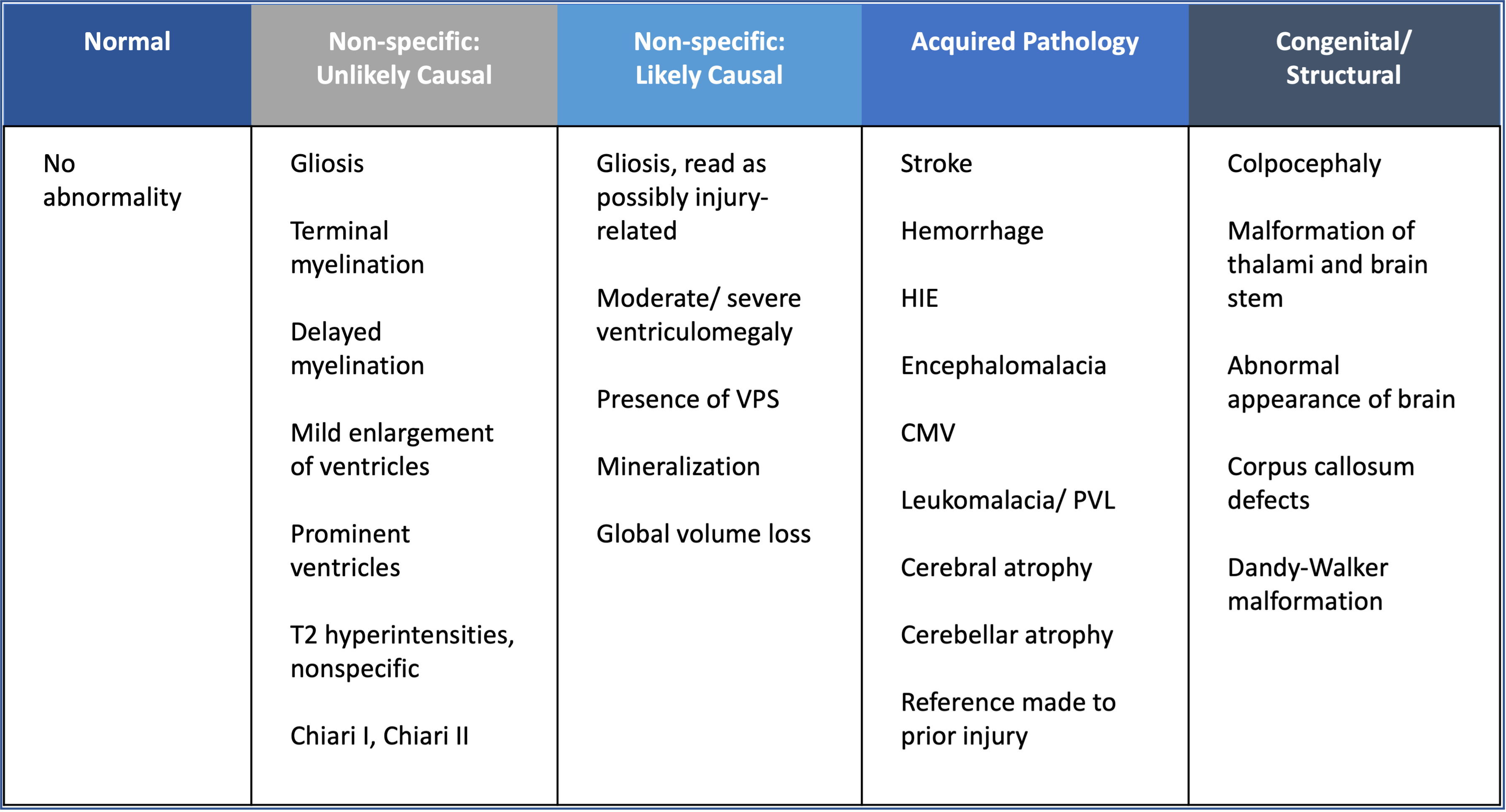
.png)
.png)
