Neonatal Neurology: Clinical Research
Neonatal Neurology 3: Clinical 3
176 - Association between hemodynamic instability with adverse short and long term outcomes in neonatal hypoxic ischemic encephalopathy
Publication Number: 176.137
- TY
Telford Yeung, MD PhD
Neonatologist
University of Windsor
Windsor, Ontario, Canada
Presenting Author(s)
Background:
Hypoxic-ischemic encephalopathy (HIE) can result in myocardial dysfunction or acute pulmonary hypertension that requires vasoactive support. In these infants with hemodynamic instability, additional brain injury can occur due to fluctuations in blood pressure and perfusion. However, there is limited data regarding the association between hemodynamic support and adverse short-term outcomes in infants with HIE.
Objective:
To assess the relationship between hemodynamic instability requiring vasoactive medications in infants with HIE undergoing therapeutic hypothermia (TH) and moderate to severe brain injury and neurodevelopmental outcomes.
Design/Methods:
We conducted a retrospective cohort study of infants greater than 35 weeks’ gestational age (GA) diagnosed with HIE who were managed by TH at quaternary level neonatal intensive care unit between January 2015 and December 2019. Patient demographics as well as perinatal and postnatal data were retrieved from electronic medical records. Brain MRI images were reviewed and scored using the Weeke scoring system. Neurodevelopment was assessed by Bayley assessments at 18 months. Clinical and radiological data were analyzed and compared between neonates who did not require inotropes/vasopressors (Group I) versus those who required inotropes/vasopressors (Group II). The association between inotropic support on MRI and Bayley scores was determined using logistic regression with modified Sarnat stage and seizures as covariates.
Results:
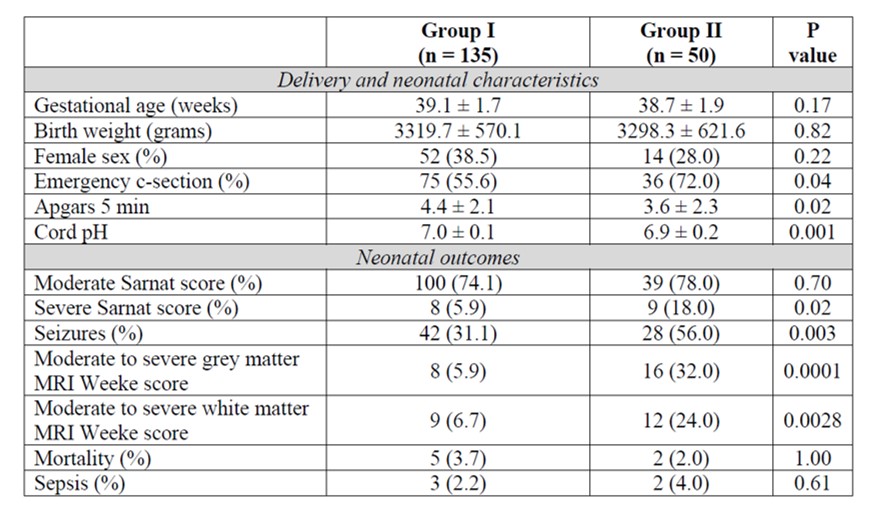
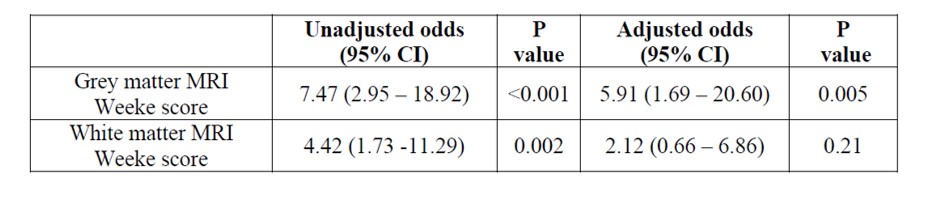
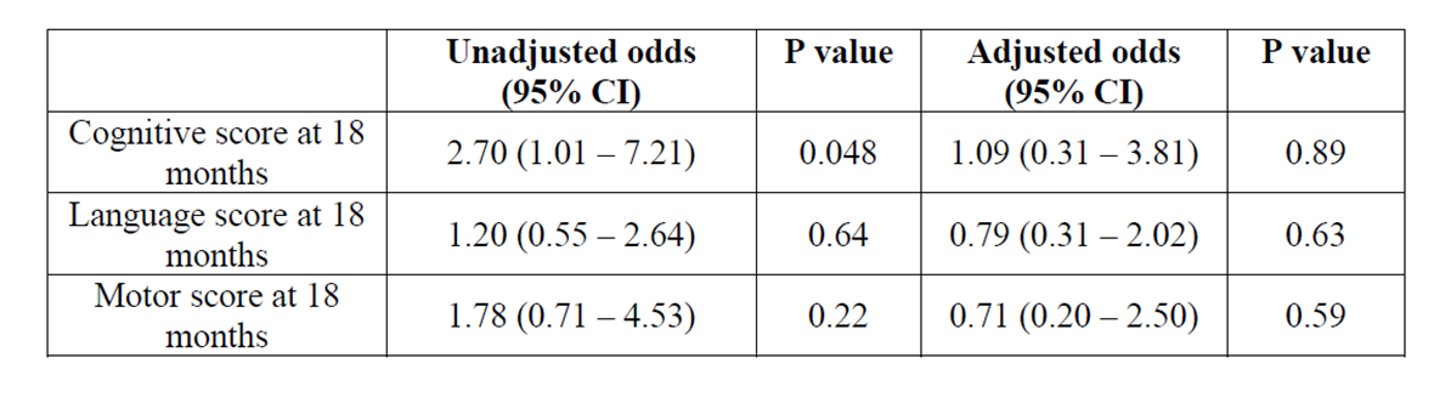
185 infants were included with 135 infants in group I and 50 infants in group II. The incidence of severe HIE and seizures were greater in group II compared to Group I (Table 1). Infants who required inotropic or vasopressor medications had worse moderate to severe grey and white matter injury on MRI. After adjustment, infants who required vasoactive medications had higher odds of moderate to severe grey matter [odds ratio (OR) 5.91; 95% confidence interval (CI) 1.69 - 20.60; P < 0.001) compared to those who did not require hemodynamic support (Table 2). However, there were no differences in neurodevelopmental impairment at 18-24 months between groups (Table 3).
Conclusion(s):
Compared to hemodynamically stable infants with HIE undergoing TH, neonates who required inotropic support had higher odds of moderate to severe grey matter brain injury on MRI but did not differ on neurodevelopmental outcomes at 18-24 months. Future studies can include the delineation of time specific BP targets during TH that are associated with favourable MRI scores and long-term neurodevelopmental outcomes.