Neonatal Follow-up
NICU Follow Up and Neurodevelopmental 2: Neonatal Growth, Nutrition and the Brain
218 - Risk of Obesity and Differential Adiposity Distribution in Adolescents Born Preterm with Very Low Birth Weight Compared to Term-born Peers
Publication Number: 218.144

Andrew M. South, MD, MS (he/him/his)
Associate Professor
Wake Forest School of Medicine of Wake Forest Baptist Medical Center
Winston Salem, North Carolina, United States
Presenting Author(s)
Background:
Strong evidence suggests that early-life factors such as preterm birth or very low birth weight increase the risk for cardiovascular disease. However, it remains unknown whether these early-life factors increase the risk of obesity, a cardiovascular risk factor, in part because studies to date have predominantly defined obesity based on body mass index.
Objective:
Investigate if adolescents born preterm with very low birth weight have a higher risk of altered adiposity distribution compared to term-born peers.
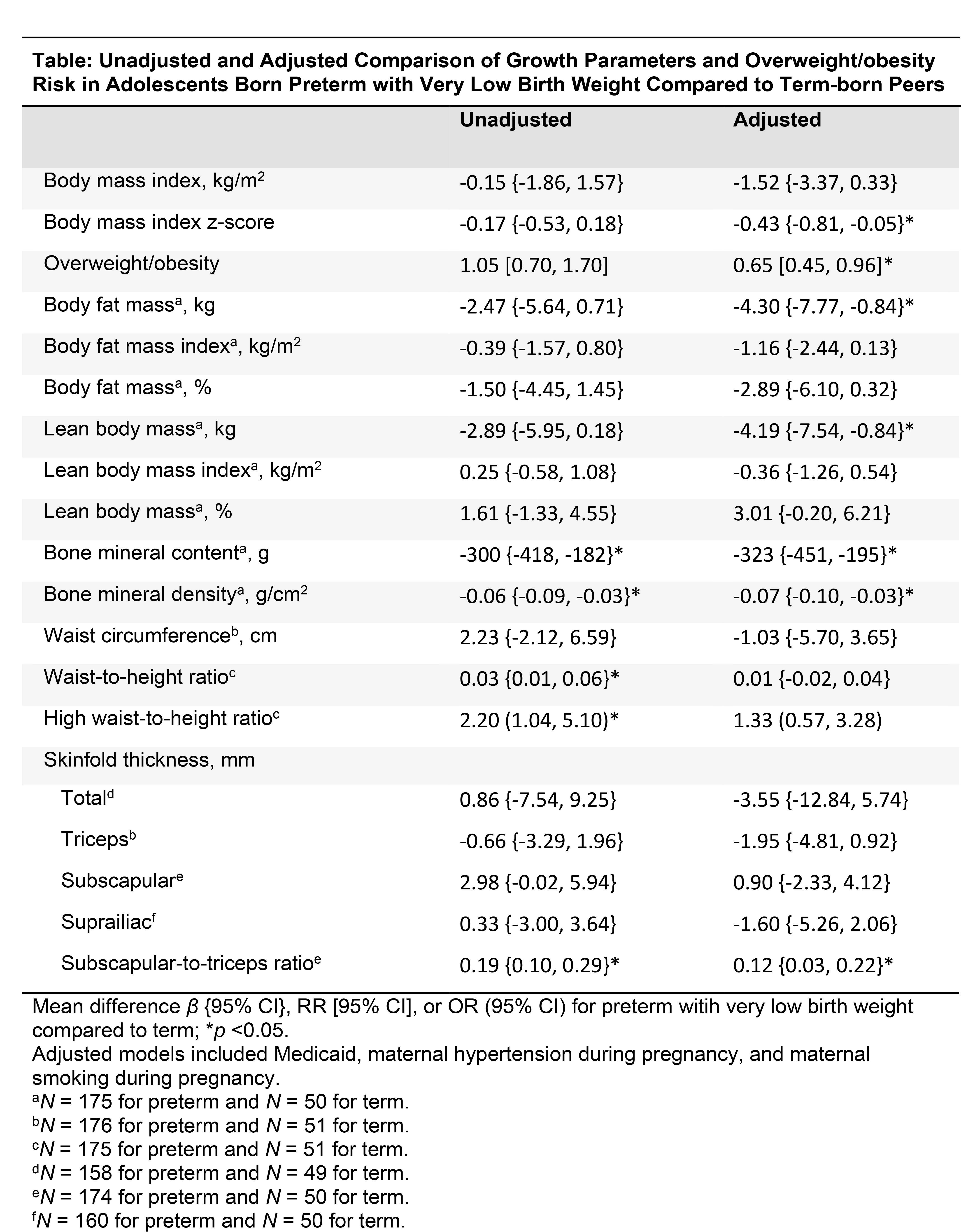
Design/Methods: Cross-sectional analysis of data from the Prenatal Events-Postnatal Consequences study, a prospective cohort of 177 individuals born preterm (< 37 weeks’ gestation) with very low birth weight (< 1.5 kg) and 51 term-born peers with birth weight ≥2.5 kg. Individuals with major congenital anomalies, genetic syndromes, or major health conditions were excluded. Perinatal data were obtained via parental report and review of health records and research databases. Participants’ height, weight, waist circumference, skinfold thickness, and DEXA body composition were measured at 14 years of age. We calculated body mass index z-scores and defined overweight/obesity as body mass index ≥85th percentile for age and sex. We estimated the preterm-term differences in overweight/obesity prevalence and adiposity distribution with multivariable generalized linear models with a directed acyclic graph-informed adjustment set containing maternal hypertension during pregnancy, maternal smoking during pregnancy, and use of Medicaid at age 14 years.
Results:
The two groups had similar proportions of being born small for gestational age (preterm 10.1%, term 11.5%). Compared to term, youth born preterm with very low birth weight had 35% lower risk of overweight/obesity (RR 0.65, 95% CI 0.45 to 0.96) and lower body fat mass, lean body mass, bone mineral content, and bone mineral density, but higher skinfold thickness (β 0.12 mm, 95% CI 0.03 to 0.22) (Table).
Conclusion(s): Youth born preterm with very low birth weight had smaller body size and a lower risk of overweight or obesity compared to term-born peers, but may have altered central adiposity. Our results highlight the importance of accurately measuring adiposity distribution rather than relying on indirect measures such as body mass index to assess for programmed alterations to adiposity.