Neonatal Quality Improvement
Neonatal Quality Improvement 1
654 - Improving the discharge process for well newborns
Publication Number: 654.138
- KI
Kelechi Ikeri, MD
Adjunct Assistant Professor
University of South Alabama Children's and Women's Hospital
Mobile, Alabama, United States
Presenting Author(s)
Background:
Hospital discharge of healthy newborns is a complex process that requires careful co-ordination. In our center, providers expressed dissatisfaction with discharge delays in the mother-baby unit especially during periods of high unit census resulting in bed unavailability. On the day of discharge, only 0.5% of healthy newborns had discharge orders placed before 10 am, time for attending rounds.
Objective:
To increase percent of discharge orders placed by 10 a.m. from 0.5% to 10% by 6months (March 2022).
Design/Methods:
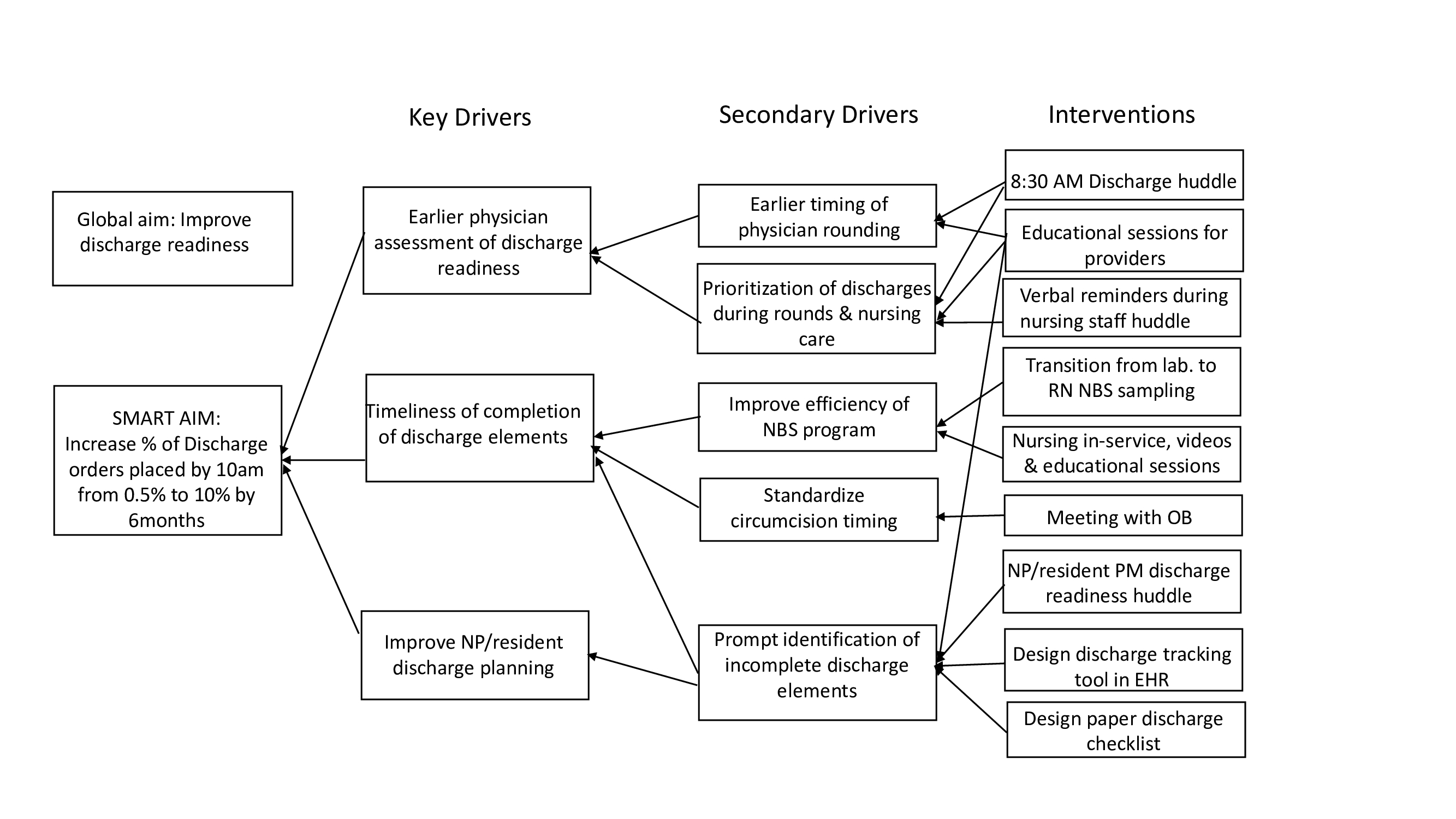
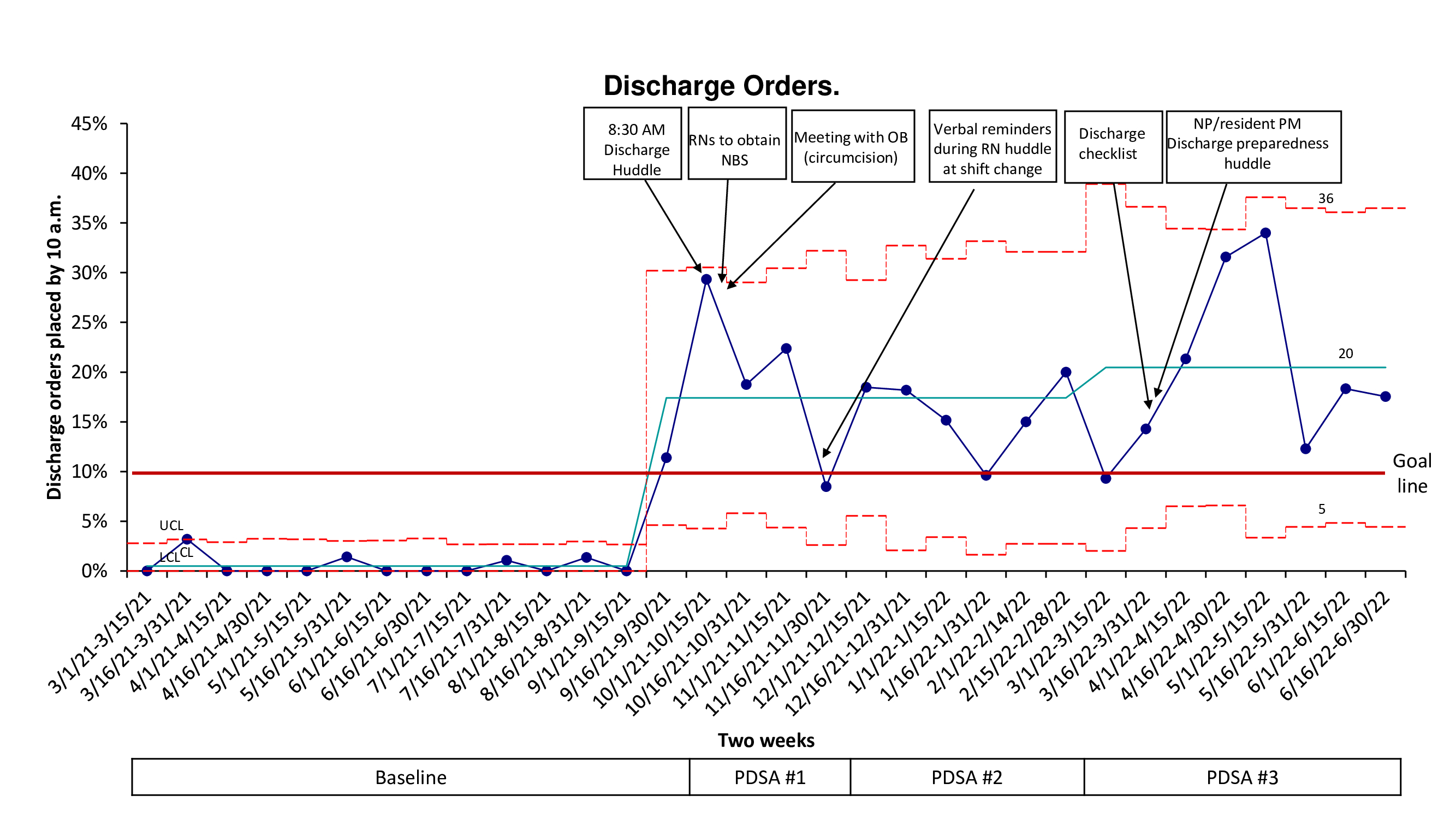
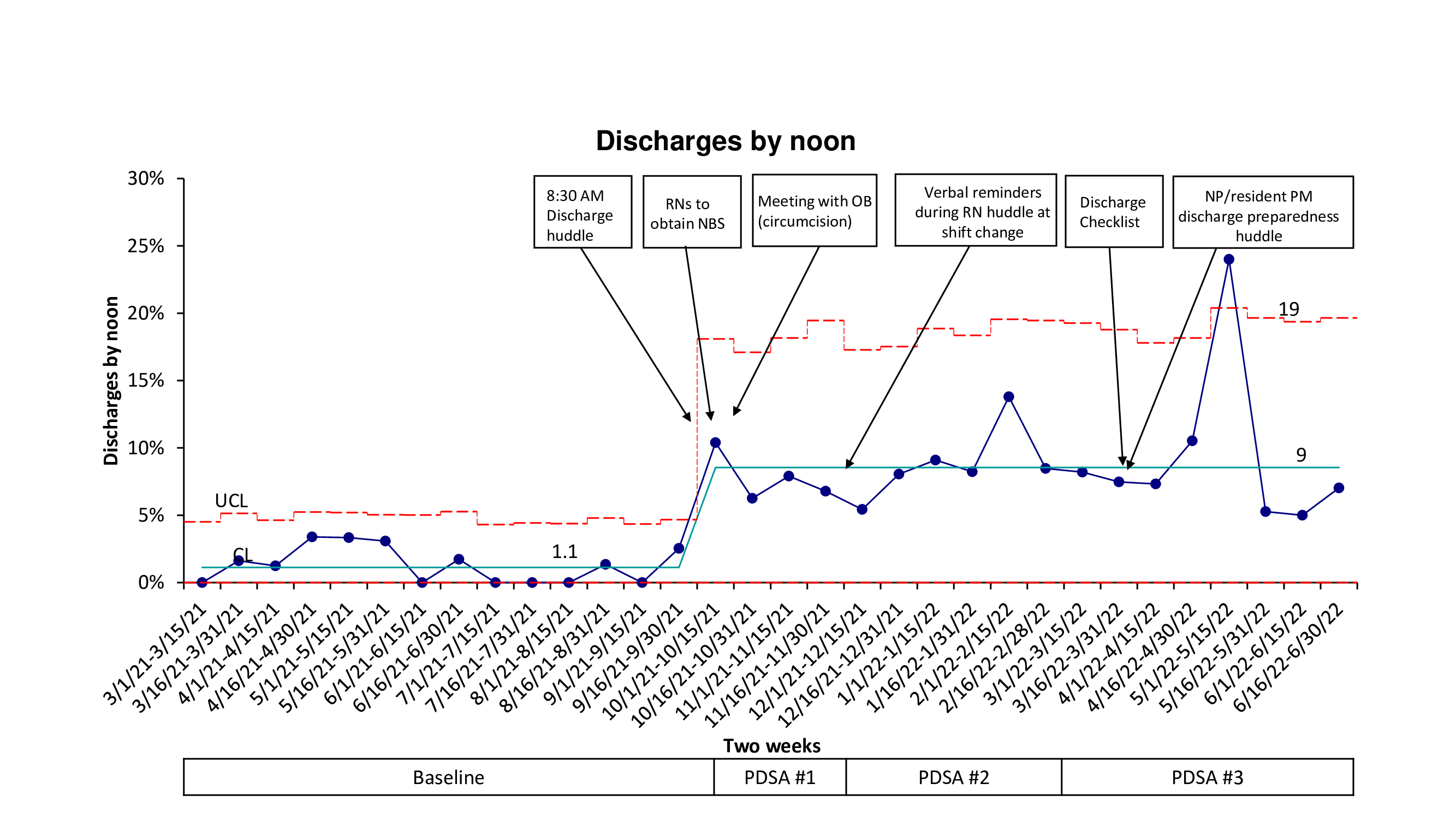
This initiative was conducted in an academic Level 1 Newborn Nursery covered by pediatric residents (2500 deliveries per year). Baseline data from March 2021-September 2021were reviewed. We identified that late physician rounding time (10 am), and inconsistencies in the newborn screening (NBS) and circumcision processes were reasons for delays. Key drivers were identified (fig 1). Starting October 2022, we implemented an 8:30 a.m. physician discharge huddle and designed a baby-bundle to facilitate finalization of all discharge screening elements by 36 hours of age. Plan-Do-Study-Act model for improvement was used. We aimed to incorporate parental preferences into discharge timing. Outcome measures were percent of discharge orders placed by 10 a.m. (discharge readiness) (fig 2) and percent of newborns discharged by noon (fig 3). Process measures were percent of NBS specimens collected and circumcisions performed before 10 a.m. Postponement of late discharges till the following morning could artificially improve early morning discharge metric. Thus, our balancing measure was percent of infants who were discharged >48hrs if delivered vaginally, and >72hrs if delivered by cesarean section (C-section). Process and outcome measures are represented on P-charts.
Results:
Baseline and improvement data were collected for 2323 newborns from March 2021 to June 2022. Our aim was exceeded as discharge orders placed by 10 a.m. improved from 0.5 % to 20%. Newborn discharges by noon increased from 1.1 % to 9 %. By 10a.m., percent of NBS specimens collected improved from 56 % to 98 % and circumcision rates increased from 66 % to 88 %. Special cause variation was detected in all outcome and process measures. Postpartum hospital days were not increased (75% to 72% of infants stayed >48hrs if vaginal delivery, 74% to 71%, if delivered by c-section).
Conclusion(s):
Accommodating parental discharge preferences by attaining newborn discharge readiness early in the day can be accomplished even in academic institutions that rely on physicians in-training for completion of discharge process.