Back
Background: Pediatric emergency department (PED) visits decreased markedly during the early part of the COVID-19 pandemic. However, little is known about differences in patient demographic characteristics, visit acuity, and diagnoses before and during the pandemic at a practice level.
Objective: To compare characteristics of PED visits before and during the pandemic from a single large urban primary care practice.
Design/Methods: We conducted a retrospective chart review of PED visits for patients from a large academic primary care practice, both located within the state’s only children’s hospital. We included patients 0-17 years old within two time periods: 5/1/2019-3/1/2020 for “pre-pandemic,” and 5/1/2020-3/1/2021 for “early-pandemic”. We collected demographic information, chief complaint, diagnosis code, level of acuity, and disposition. Chief complaint and diagnosis code were used to group visits into medical versus psychiatric. We used counts/percentages, mean/SD, and mean/IQR to describe variables, and Fisher's exact and Wilcoxon rank-sum tests to compare variables between the two time periods, further evaluating the data by stratifying by age groups.
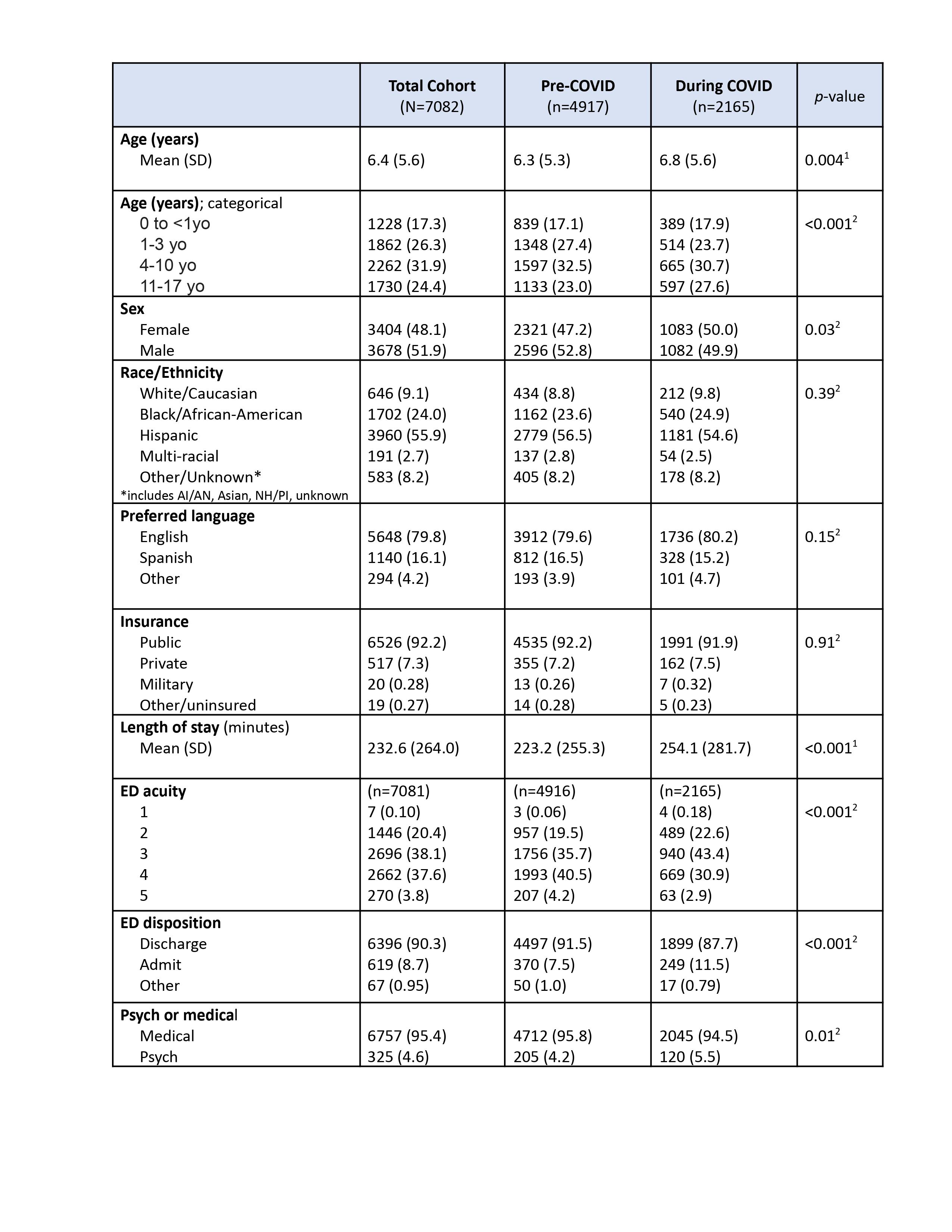
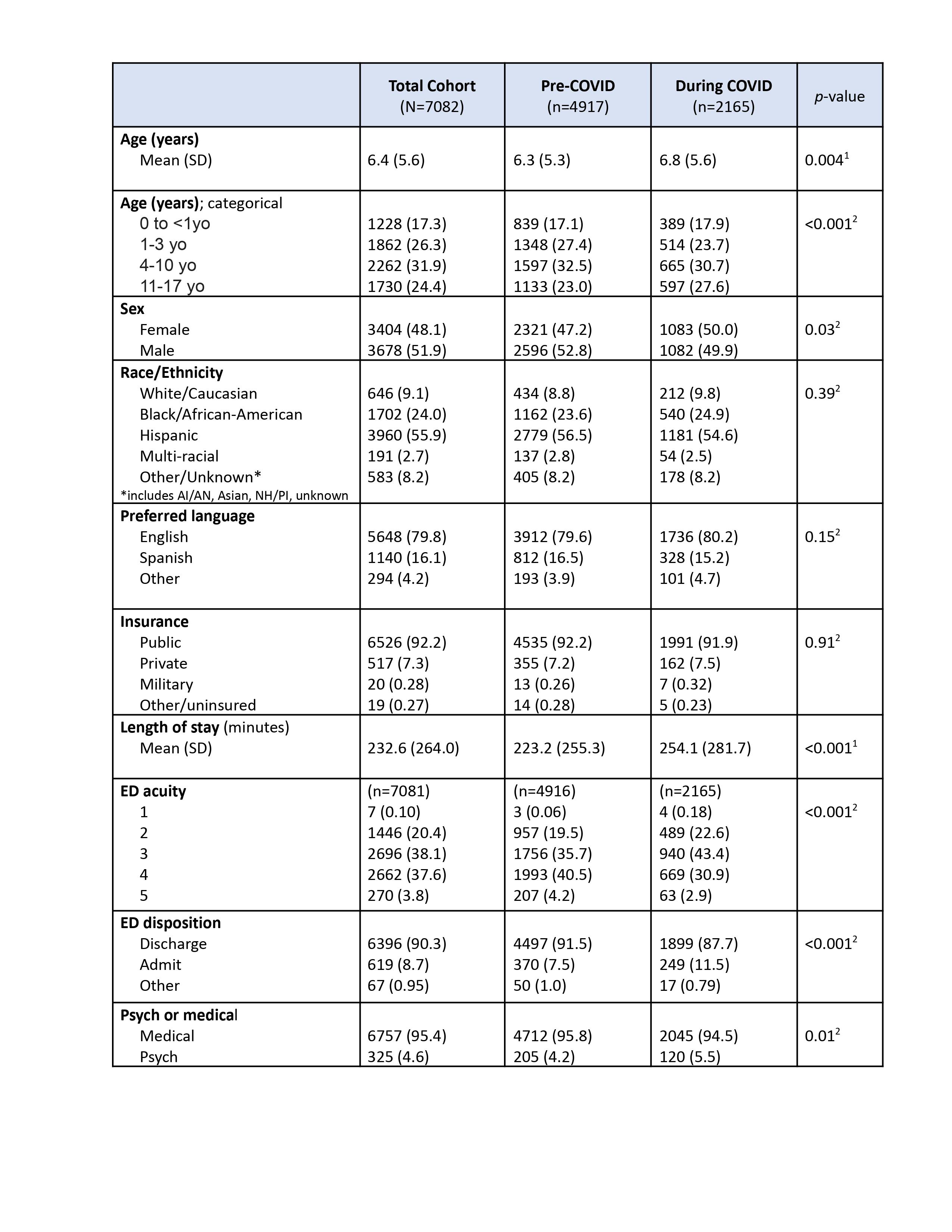
Results: We reviewed 5,134 pre-pandemic and 2,230 early pandemic PED visits from our practice. There were no significant differences in insurance, preferred language or race/ethnicity (Table 1). Children seen during the early pandemic were significantly older, had longer lengths of stay, and were more likely to be admitted than prior to the pandemic. Visits for psychiatric complaints increased significantly during the pandemic. When stratifying by age, level of acuity increased significantly in children 1 year and older, and length of stay increased significantly in children 4-17 years old during the pandemic vs pre-pandemic. Admission rates increased significantly in children 4-10 years old (Table 2).
Conclusion(s): While some primary care offices stopped seeing “sick” visits, this medical home maintained both in person and telehealth access. This access may have mitigated racial disparities seen in other studies. However, fear of exposure to COVID-19 may explain the higher level of acuity due to delay in seeking care. The proportion of mental health visits increased significantly during the pandemic which likely reflected high stress levels affecting the pediatric population.
.jpg)
Emergency Medicine: All Areas
Emergency Medicine 4
72 - Pediatric emergency department utilization before and during the COVID-19 pandemic by an urban academic primary care practice
Friday, April 28, 2023
5:15 PM – 7:15 PM ET
Poster Number: 72
Publication Number: 72.112
Publication Number: 72.112
Bruna Olson, Baystate Children's Hospital, Wilbraham, MA, United States; Nadya I. Rivera Gelabert, University of Puerto Rico School of Medicine, Bayamon, N/A, Puerto Rico; Shuba Kamath, The Warren Alpert Medical School of Brown University/Hasbro Children's Hospital, Barrington, RI, United States; Allison Heinly, The Warren Alpert Medical School of Brown University/Hasbro Children's Hospital, Providence, RI, United States; Natalia Golova, Hasbro Children's Hospital at Rhode Island Hospital, Providence, RI, United States; Phinnara Has, Rhode Island Hospital, Providence, RI, United States; Alison Riese, The Warren Alpert Medical School of Brown University/Hasbro Children's Hospital, Cranston, RI, United States

Bruna Olson, MD (she/her/hers)
Pediatric Emergency Fellow
Baystate Children's Hospital
Wilbraham, Massachusetts, United States
Presenting Author(s)
Background: Pediatric emergency department (PED) visits decreased markedly during the early part of the COVID-19 pandemic. However, little is known about differences in patient demographic characteristics, visit acuity, and diagnoses before and during the pandemic at a practice level.
Objective: To compare characteristics of PED visits before and during the pandemic from a single large urban primary care practice.
Design/Methods: We conducted a retrospective chart review of PED visits for patients from a large academic primary care practice, both located within the state’s only children’s hospital. We included patients 0-17 years old within two time periods: 5/1/2019-3/1/2020 for “pre-pandemic,” and 5/1/2020-3/1/2021 for “early-pandemic”. We collected demographic information, chief complaint, diagnosis code, level of acuity, and disposition. Chief complaint and diagnosis code were used to group visits into medical versus psychiatric. We used counts/percentages, mean/SD, and mean/IQR to describe variables, and Fisher's exact and Wilcoxon rank-sum tests to compare variables between the two time periods, further evaluating the data by stratifying by age groups.
Results: We reviewed 5,134 pre-pandemic and 2,230 early pandemic PED visits from our practice. There were no significant differences in insurance, preferred language or race/ethnicity (Table 1). Children seen during the early pandemic were significantly older, had longer lengths of stay, and were more likely to be admitted than prior to the pandemic. Visits for psychiatric complaints increased significantly during the pandemic. When stratifying by age, level of acuity increased significantly in children 1 year and older, and length of stay increased significantly in children 4-17 years old during the pandemic vs pre-pandemic. Admission rates increased significantly in children 4-10 years old (Table 2).
Conclusion(s): While some primary care offices stopped seeing “sick” visits, this medical home maintained both in person and telehealth access. This access may have mitigated racial disparities seen in other studies. However, fear of exposure to COVID-19 may explain the higher level of acuity due to delay in seeking care. The proportion of mental health visits increased significantly during the pandemic which likely reflected high stress levels affecting the pediatric population.
.jpg)
