Back
Background: Teaching clinics care for a high proportion of underserved patients (Serwint 2006). Resident patients have worse chronic disease and preventive screening outcomes compared to non-residents patients (Amat 2021, Essien 2019). Continuity is a key driver for improved preventive care (Flores 2008) and reduction of high-cost health encounters (Enlow 2017, Tom 2010). After a chart review revealed our resident continuity rates dropped from 30% in 2018 (n = 68) to 16% in 2021 (n = 71), we launched a quality improvement (QI) initiative.
Objective: To improve resident patient continuity across 3 teaching clinics from 16% to 36% by June 2022.
Design/Methods: Residents and preceptors at 3 clinics reviewed resident schedules using the “continuity for physician” formula (Darden 2001): proportion of patients on a provider’s schedule that they have seen before. Residents and preceptors used interviews of patient service representatives to map scheduling processes. They brainstormed key drivers for continuity, identified potential interventions and ranked interventions by impact/feasibility (Figure 1). To explore patient-level outcomes that may be impacted by continuity, we engaged key primary care stakeholders with access to validated data dashboards. The following metrics were obtained: well visits by 15 months old and immunization completion at 2 years old.
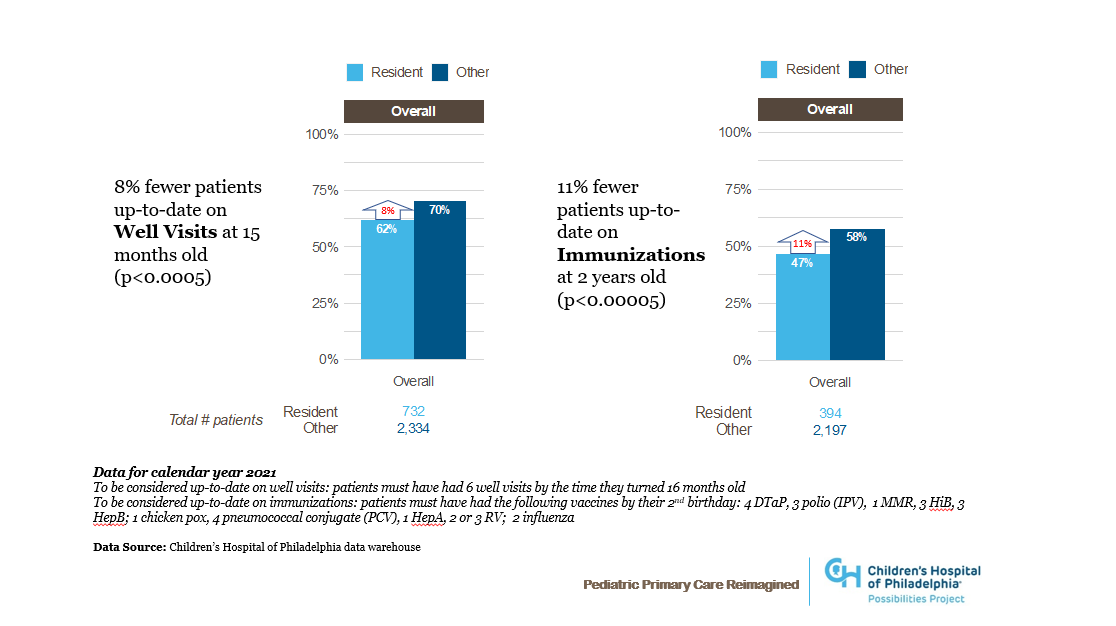
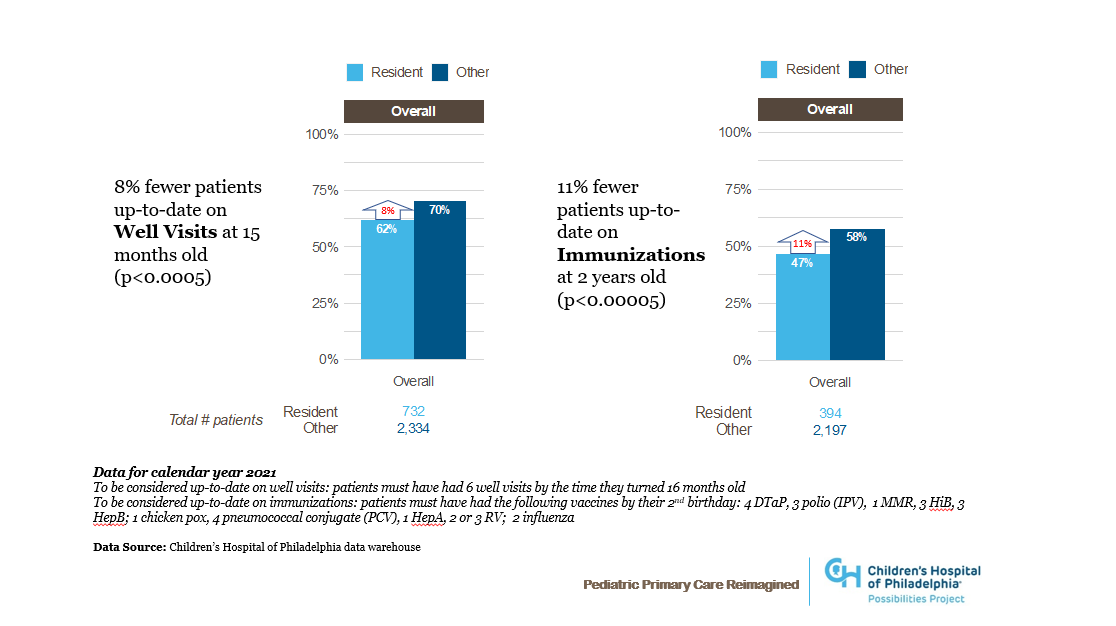
Results: Our first interventions were to open resident clinic schedules earlier (4 months vs 3 months) and create resident teams to collectively care for a shared group of patients (March 2022). Our resident continuity rate improved with a shift of 8 points above the median beginning in September 2021 (Figure 2). Patient level data from 2021, stratified by resident and non-resident provider, revealed disparities in care: patients with resident providers had lower well visit completion rates at 15 months old and lower immunization completion at 2 years old (Figure 3).
Conclusion(s): Teaching clinics often care for a marginalized patient population. Our QI initiative confirmed healthcare disparities among patients with resident providers, with poor continuity as a potential contributor. After opening resident schedules earlier and introducing a team-based approach, our data showed improved continuity with a shift above baseline. Patient-level outcomes data for 2022 are not yet available. Future potential changes include placing caps on resident patient panels and significant operational restructuring to better support resident patients.
.png)
.png)
Quality Improvement/Patient Safety: Primary & Subspecialty Outpatient Quality Improvement
QI 2: Screening in Primary Care
693 - Disparities and Barriers Identified through a Longitudinal Initiative to Improve Resident-Patient Continuity
Friday, April 28, 2023
5:15 PM – 7:15 PM ET
Poster Number: 693
Publication Number: 693.152
Publication Number: 693.152
Elizabeth Kuhn, Childrens Hospital of Philadelphia, Philadelphia, PA, United States; Ami Patel, Childrens Hospital of Philadelphia, Philadelphia, PA, United States; Prerana Chatty, CHOP, Philadelphia, PA, United States; Abrar Alabdulhadi, children's hospital of philadephia, Philadelphia, PA, United States; Nicholas santaniello, Childrens Hospital of Philadelphia, Philadelphia, PA, United States; Christine Cummings, Childrens Hospital of Philadelphia, Philadelphia, PA, United States; Beth Rezet, Childrens Hospital of Philadelphia, Havertown, PA, United States; Elena Huang, Children's Hospital of Philadelphia, Philadelphia, PA, United States

Elizabeth Kuhn, MD (she/her/hers)
Chief Resident
Childrens Hospital of Philadelphia
Philadelphia, Pennsylvania, United States
Presenting Author(s)
Background: Teaching clinics care for a high proportion of underserved patients (Serwint 2006). Resident patients have worse chronic disease and preventive screening outcomes compared to non-residents patients (Amat 2021, Essien 2019). Continuity is a key driver for improved preventive care (Flores 2008) and reduction of high-cost health encounters (Enlow 2017, Tom 2010). After a chart review revealed our resident continuity rates dropped from 30% in 2018 (n = 68) to 16% in 2021 (n = 71), we launched a quality improvement (QI) initiative.
Objective: To improve resident patient continuity across 3 teaching clinics from 16% to 36% by June 2022.
Design/Methods: Residents and preceptors at 3 clinics reviewed resident schedules using the “continuity for physician” formula (Darden 2001): proportion of patients on a provider’s schedule that they have seen before. Residents and preceptors used interviews of patient service representatives to map scheduling processes. They brainstormed key drivers for continuity, identified potential interventions and ranked interventions by impact/feasibility (Figure 1). To explore patient-level outcomes that may be impacted by continuity, we engaged key primary care stakeholders with access to validated data dashboards. The following metrics were obtained: well visits by 15 months old and immunization completion at 2 years old.
Results: Our first interventions were to open resident clinic schedules earlier (4 months vs 3 months) and create resident teams to collectively care for a shared group of patients (March 2022). Our resident continuity rate improved with a shift of 8 points above the median beginning in September 2021 (Figure 2). Patient level data from 2021, stratified by resident and non-resident provider, revealed disparities in care: patients with resident providers had lower well visit completion rates at 15 months old and lower immunization completion at 2 years old (Figure 3).
Conclusion(s): Teaching clinics often care for a marginalized patient population. Our QI initiative confirmed healthcare disparities among patients with resident providers, with poor continuity as a potential contributor. After opening resident schedules earlier and introducing a team-based approach, our data showed improved continuity with a shift above baseline. Patient-level outcomes data for 2022 are not yet available. Future potential changes include placing caps on resident patient panels and significant operational restructuring to better support resident patients.
.png)
.png)
