Hospital Medicine: Hospital Medicine Quality Improvement
Hospital Medicine 2
759 - De-implementing umbilical cord toxicology testing at a community hospital site
Publication Number: 759.12
- SO
Sharon Ostfeld-Johns, MD (she/her/hers)
Assistant Professor of Clinical Pediatrics and Assistant Professor of Medicine
Yale-New Haven Children's Hospital
New Haven, Connecticut, United States
Presenting Author(s)
Background:
In the absence of clear evidence-based guidelines, most hospitals establish their own protocols for newborn drug testing. There is no established preferred testing modality. Meconium testing was developed as an adjunct to urine drug testing, and recently, more expensive umbilical cord drug (UCD) testing was studied to evaluate substance exposure throughout the latter stages of pregnancy. In both cases, the reasons cited for testing have unclear relevance to the clinical care of newborns with prenatal substance exposure. Moreover, many studies have shown that over-utilization of drug testing introduces bias and racism.
Within our large health system with over 10,000 annual births in the Northeast, newborns are cared for at 4 sites. Urine toxicology testing is performed at 3 sites and UCD testing at one of the community hospitals.
Objective:
We sought to understand the reasons for ordering UCD tests, and how the results of the tests were interpreted. From this we would be able to extrapolate the value of UCD testing in newborn care. Our hypothesis was that test results rarely provided actionable information, either for optimal clinical care or disposition decision-making.
Design/Methods:
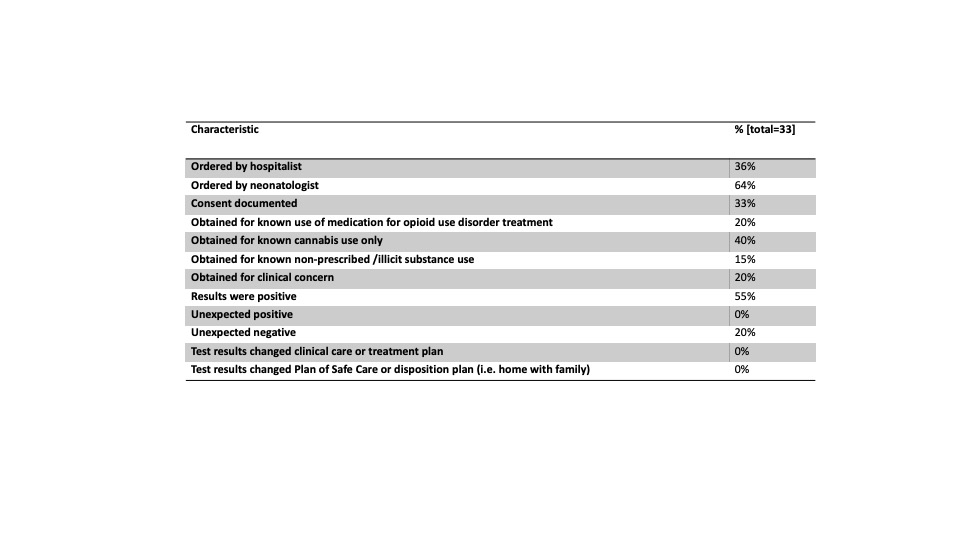
Retrospective chart review included a total of 33 infants who had UCD tests over a 3-year period (2019-2021). Charts were assessed for reasons for ordering UCD tests including: 1) known maternal history of substance use during pregnancy, 2) known treatment for opioid use disorder, or 3) clinical concerns. We evaluated whether test results were in accordance with expectations, and if the results prompted a change in clinical care or the plan of safe care after the newborn hospitalization.
Results:
Of the 33 infants with UCD tests, none had an “unexpectedly positive” result – meaning that none of the results demonstrated substance exposure that was previously unknown. Tests therefore never resulted in changes to clinical care or the disposition plan.
Conclusion(s):
Umbilical cord drug tests did not add value to care of newborns based on a 3-year experience at one community site within a large health system. Tests did not provide clinically actionable information, or information that is necessary for ensuring safety in newborn disposition planning. As a result our care team opted to de-implement the use of UCD tests and use urine tests when toxicology testing is clinically indicated. De-implementation of the testing program will reduce cost and likely improve equity. Larger studies should be undertaken to demonstrate that these tests, along with their equivalent – meconium tests - do not improve the care of newborns.