Telemedicine/EHR/Medical Informatics
Telemedicine/EHR/Medical Informatics 1
728 - A Novel Method to Screen for Urinary Tract Infections with Artificial Intelligence and Smartphone Images
Publication Number: 728.154
Therese Canares, MD, MBA (she/her/hers)
Assistant Professor
Johns Hopkins University
Baltimore, Maryland, United States
Presenting Author(s)
Background:
Urinary tract infections (UTIs) are a common condition treated via telehealth. Symptoms of a simple cystitis in a low risk adult female are often treated with antibiotics, without a urinalysis. However, children and adolescents require urine testing to confirm a UTI, which limits options for remote care. Predictive models using artificial intelligence (AI) may risk stratify UTIs in children, although none exist currently.
Objective:
Our aim is to demonstrate feasibility of an AI algorithm to predict a UTI using smartphone images of a urine sample.
Design/Methods:
This cross-sectional study was conducted at urban, tertiary care hospital, May ‘21-July ‘22, with IRB approval. Urine samples from the pediatric emergency department or core laboratory were included if a urinalysis or urine culture was performed, collected on a convenience basis. The ground truth was defined as Positive UTI: >100,000 colony forming units (CFU)/mL in a clean catch or > 10,000 CFU/mL in a catheter specimen; Negative UTI: no growth from culture or negative nitrite/leukocyte esterase on urinalysis/dipstick.
The urine specimen images were recorded on a smartphone. The images were inputs into a convolutional neural network; the output was a binary prediction of positive/negative for UTI. 250 urine specimens were recorded, and 5-11 images per specimen comprised the dataset. The dataset was randomly divided for each phase of algorithm development: ~63% (1582 images) for training, ~16% (399 images) for validation, and ~20% (500 images) for testing. Results of the AI algorithm characteristics were obtained with 5-fold cross validation. Performance of the AI is reported on the testing image dataset.
Outcomes were sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) of the AI algorithm.
Results:
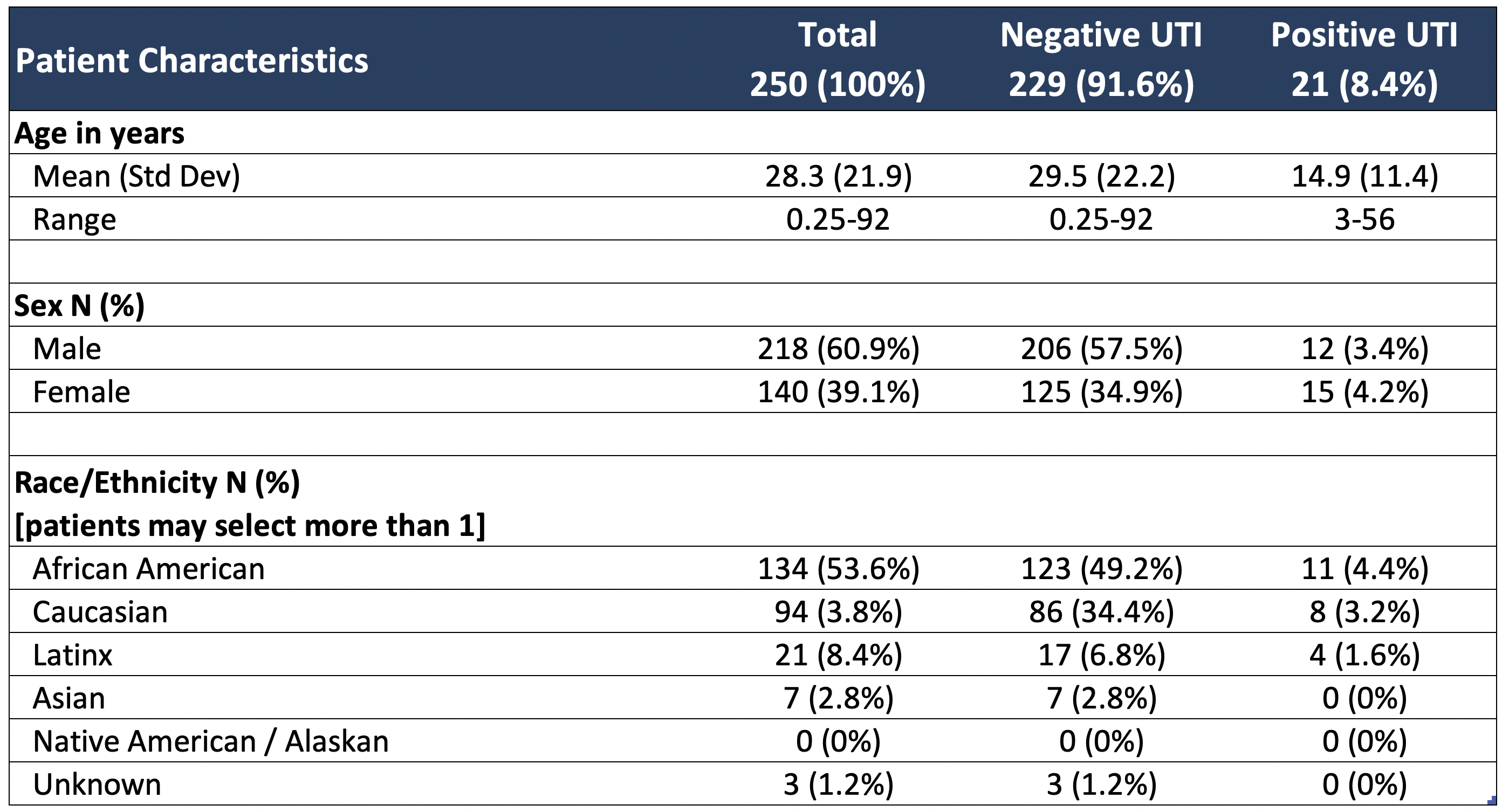
Patient characteristics from the 250 urine specimens are noted in Table 1. The overall prevalence of UTI was 8.4%. The average characteristics of the AI algorithm are: sensitivity 45.3%, specificity 90.2%, positive predictive value 33.6%, and negative predictive value 93.6%.
Conclusion(s):
This study demonstrates feasibility of an AI algorithm to predict UTI in a pediatric and adult population using a smartphone image. Limitations were a relatively small dataset, imbalanced toward negative samples. Future studies to enhance AI performance will increase the sample size to train the predictive model, and limit to patients who present with acute symptoms of cystitis. Remote UTI screening with a smartphone has implications as a clinical decision support tool for telehealth.