Back
Background: Addressing social needs such as food insecurity (FI) in healthcare has become a priority with the Affordable Care Act’s implementation. Yet there are limited experiential learning modalities equipping medical students to effectively address FI.
Objective: To establish a novel curriculum for medical students that expands their knowledge surrounding FI and increases their confidence in referring patients to community resources.
Design/Methods: Medical students from Washington, DC who volunteered to become Patient Navigators were trained on screening and intervening techniques to address FI through the local context, and primary care providers referred patients who screened positive for FI to the Patient Navigators' services. To assess the Patient Navigator experience, participating medical students completed pre- and 6-month post-surveys designed to explore knowledge about FI and community resources, confidence in referring to resources, attitudes towards patients experiencing FI, and behaviors regarding FI. Response options were 5-point Likert-type scales. We report demographics of participants and the frequency of response types, and test the difference in the pre-post distribution of response frequencies with a Fisher exact test.
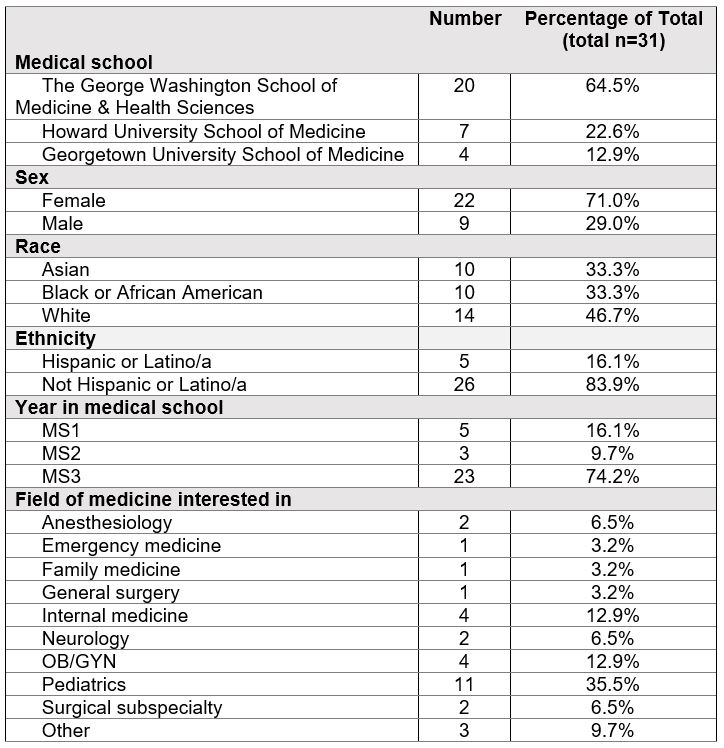
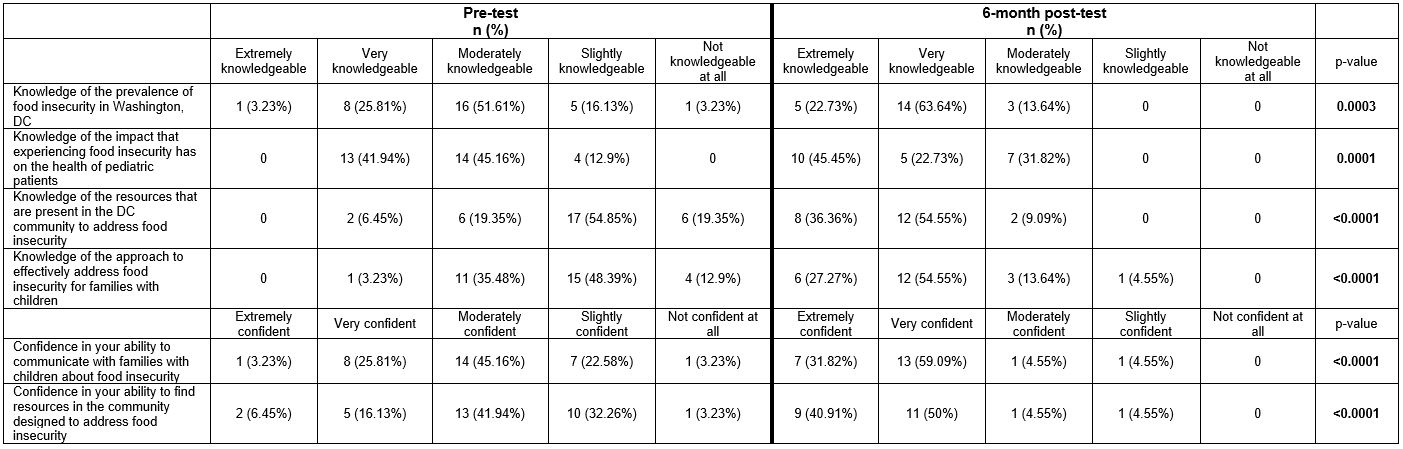
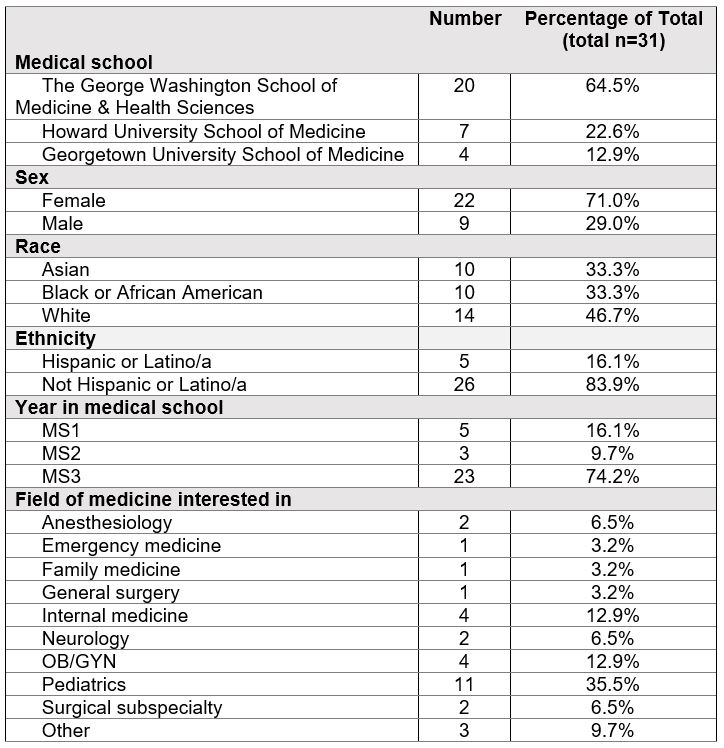
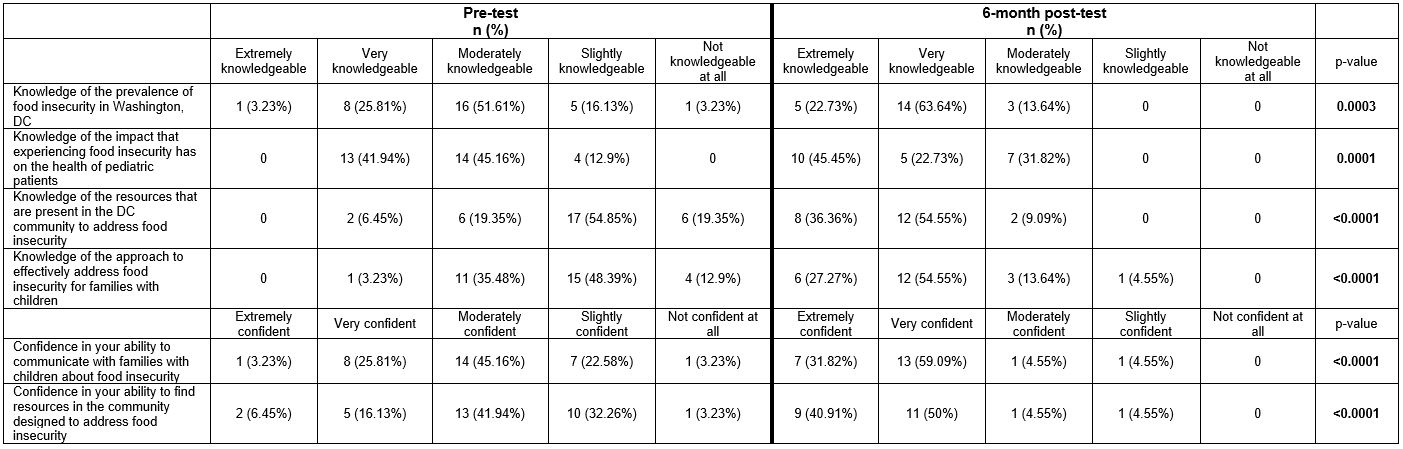
Results: Thirty-one students responded to the baseline survey and 22 responded to the 6-month survey. Demographics of baseline respondents can be found in Table 1. The majority of students provided resources to 3-5 (28.6%) or 6-10 (23.8%) families. Compared to baseline, at the 6-month evaluation mark, a significantly larger proportion of students reported being extremely or very knowledgeable about the prevalence of food insecurity in DC, the health impacts of FI, the availability of local FI resources, and approaches to effectively address FI (all p< 0.01). A larger proportion of students also reported being very confident or confident in communicating with families about FI, finding resources to address FI, and understanding how to refer to local/regional/national food programs (all p< 0.01) (Table 2). On average, participants rated their overall experience as a patient navigator as 8.29 on a scale from 1-10.
Conclusion(s): In this cohort of students, our novel program that gives medical students first-hand experience was effective in increasing their knowledge related to FI and their confidence in referring families to appropriate resources. Future studies will require mixed methods analysis to explore lived experiences and more longitudinal potential changes amongst medical students.
Medical Education: Medical Student
Medical Education 2: Student 1
470 - FLiP Navigators: A mid-program evaluation of a novel food insecurity curriculum for medical students
Friday, April 28, 2023
5:15 PM – 7:15 PM ET
Poster Number: 470
Publication Number: 470.123
Publication Number: 470.123
Lauren Dzera, Children's National Health System, Washington, DC, United States; Katrina Stumbras, Children's National Health System, Washington, DC, United States; Alicia Tucker, Children's National Health System, Alexandria, VA, United States; Laura Fischer, Children's National Health System, Washington, DC, United States; Kofi Essel, Children's National Health System, Washington, DC, United States

Lauren Dzera, MD (she/her/hers)
Pediatric Resident
Children's National Health System
Washington, District of Columbia, United States
Presenting Author(s)
Background: Addressing social needs such as food insecurity (FI) in healthcare has become a priority with the Affordable Care Act’s implementation. Yet there are limited experiential learning modalities equipping medical students to effectively address FI.
Objective: To establish a novel curriculum for medical students that expands their knowledge surrounding FI and increases their confidence in referring patients to community resources.
Design/Methods: Medical students from Washington, DC who volunteered to become Patient Navigators were trained on screening and intervening techniques to address FI through the local context, and primary care providers referred patients who screened positive for FI to the Patient Navigators' services. To assess the Patient Navigator experience, participating medical students completed pre- and 6-month post-surveys designed to explore knowledge about FI and community resources, confidence in referring to resources, attitudes towards patients experiencing FI, and behaviors regarding FI. Response options were 5-point Likert-type scales. We report demographics of participants and the frequency of response types, and test the difference in the pre-post distribution of response frequencies with a Fisher exact test.
Results: Thirty-one students responded to the baseline survey and 22 responded to the 6-month survey. Demographics of baseline respondents can be found in Table 1. The majority of students provided resources to 3-5 (28.6%) or 6-10 (23.8%) families. Compared to baseline, at the 6-month evaluation mark, a significantly larger proportion of students reported being extremely or very knowledgeable about the prevalence of food insecurity in DC, the health impacts of FI, the availability of local FI resources, and approaches to effectively address FI (all p< 0.01). A larger proportion of students also reported being very confident or confident in communicating with families about FI, finding resources to address FI, and understanding how to refer to local/regional/national food programs (all p< 0.01) (Table 2). On average, participants rated their overall experience as a patient navigator as 8.29 on a scale from 1-10.
Conclusion(s): In this cohort of students, our novel program that gives medical students first-hand experience was effective in increasing their knowledge related to FI and their confidence in referring families to appropriate resources. Future studies will require mixed methods analysis to explore lived experiences and more longitudinal potential changes amongst medical students.