Telemedicine/EHR/Medical Informatics
Telemedicine/EHR/Medical Informatics 1
740 - Use of Design Thinking and Human Factors Approach to Improve Situation Awareness in the Pediatric ICU
Publication Number: 740.154

Matthew W. Zackoff, MD, MEd (he/him/his)
Assistant Professor
Cincinnati Children's Hospital Medical Center
Cincinnati, Ohio, United States
Maya Dewan, MD, MPH (she/her/hers)
Assistant Professor
Cincinnati Children's Hospital Medical Center
Cincinnati, Ohio, United States
Presenting Author(s)
Co-Author(s)
Background:
Optimal design of a healthcare space can enhance patient safety. With a planned transition to a new clinical space for the pediatric ICU (PICU), there were concerns the new physical layout would reduce situation awareness (SA) leading to increased rates of clinical deterioration. To mitigate this we applied design thinking and human factors to address SA concerns.
Objective: To measure the impact of these changes in the new clinical space.
Design/Methods:
The clinical team collaborated with LiveWell, a design research group, to better understand the SA workflows, collect feedback from the bedside staff, pilot new signage, and design a mitigation plan prototype to improve shared and individual SA. New bedside mitigation plans were installed within the new clinical space. In addition, through team feedback from the design process we instituted color coded electronic door signs based on patient risk status. We surveyed the individual and shared SA of PICU care team trios (bedside nurses [RN], residents, and bedside respiratory therapists [RT]) for 12 months pre- and post-transition t to assess knowledge of patient risk status, reason for assigned risk status, and the mitigation plan. Each caregiver role in the patient care trio was separately surveyed about the shared patient. Their responses were compared to the unit patient status document that is reviewed twice daily by nursing and physician leadership – the gold standard for this data. Accuracy of individual SA for each care team role was expressed as percentages with statistical changes from pre- to post-transition assed through chi-squared testing.
Results:
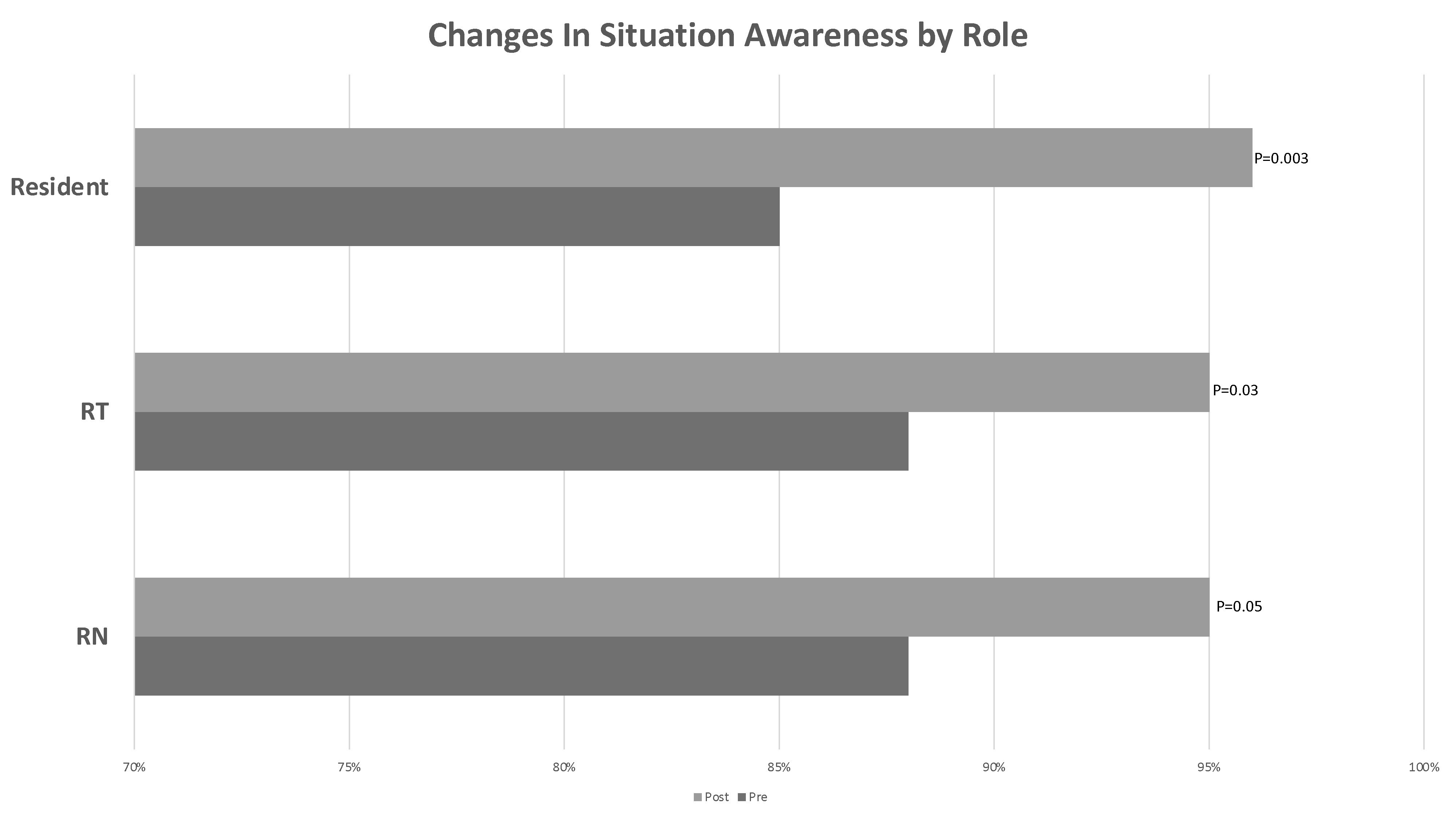
A total of 684 PICU staff were evaluated pre-transition and 312 post-transition. Shared SA for high-risk status for care teams improved from 81% to 92% (p=.006) for all patients. Accuracy of patient high-risk status by role improved from 88% to 95% (p=.05) for RNs, 85% to 96% (p=.003) for residents, and 88% to 95% (p=.03) for RTs. Shared accuracy of reason for high-risk status for care teams improved from 46% to 76% (p=.005). There was no difference in shared SA for knowledge of mitigation plan.
Conclusion(s): Using user centered design, new SA tools put into place prior to a move to a new critical care clinical space that were associated with improved individual and shared SA. These approaches may be applicable other critical care and inpatient units to improve shared SA