Child Abuse & Neglect
Child Abuse & Neglect 1
595 - Evaluating Potential Bias of CPS Referrals in Cases of Unintentional Ingestions
Friday, April 28, 2023
5:15 PM - 7:15 PM ET
Poster Number: 595
Publication Number: 595.103
Publication Number: 595.103
Gabriella Giugliano, Children's National Hospital, Washington, DC, United States; Danae L. Massengill, Children's National Hospital, Washington, DC, United States; Madhuri Uppuluri, Children's National Health System, Reston, VA, United States; Gia M. Badolato, Children's National Health System, Washington, DC, United States; Xian Zhao, Children's National Health System, Washington, DC, United States

Gabriella Giugliano, MD (she/her/hers)
PGY-3 Pediatric Resident
Children's National Hospital
Washington, District of Columbia, United States
Presenting Author(s)
Background: Unintentional ingestions (UI) are a common cause for presentation to the pediatric emergency department (PED). While UIs can result from exploratory behavior, they often happen in the setting of improper storage, neglect or abuse due to another person's deliberate administration with non-therapeutic intent. UI cases lack standardized recommendations regarding when to call Child Protective Services (CPS). This results in provider discretion, which allows for the introduction of bias to the clinical decision-making process.
Objective: Identify patient and visit level characteristics associated with CPS referral status in UI cases.
Design/Methods: This was a retrospective cross-sectional study of children ≤6 years old who presented to a large, metropolitan PED from 2015 to 2021 and were diagnosed with UI. We queried our electronic health record to identify visits with ICD-10 codes associated with abuse, neglect, ingestion, and other related terms. CPS referrals were determined by manual chart review. Bivariable and multivariable logistic regression models were used to identify patient and visit level characteristics associated with CPS referral. Socioeconomic status (SES) was classified based on zip code, the 2015 metro Child Opportunity Index data, and insurance status.
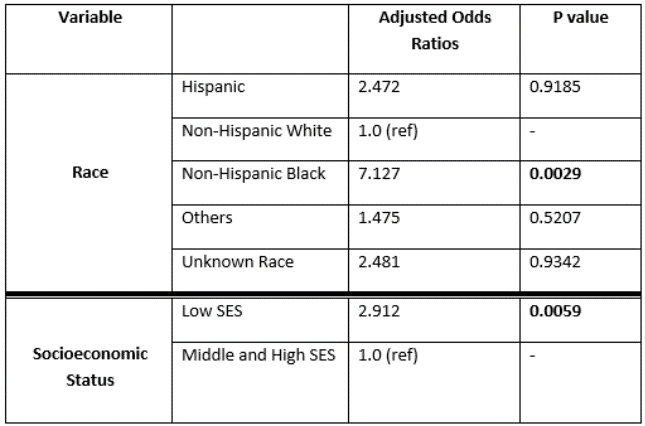
Results: Of 3,836 charts reviewed, 808 UI visits met inclusion criteria. CPS referrals were made in 109 (13.5%) visits. The majority of patients were between the ages of 1 and 2 (58.66%), non-Hispanic Black (74.01%), male (53.34%), or classified as children in low SES households (74.26%). Compared to non-Hispanic white patients, non-Hispanic Black patients had 7.1 (95% CI:1.3, 38.7) higher adjusted odds of being referred to CPS after adjusting for triage level, age, and ingestion type. Patients in the low SES group had an aOR of 2.9 (95% CI:1.4, 6.2) when compared to patients in the middle or high SES group.
Conclusion(s): Our study found that CPS referrals in UI cases occur more often in those identifying as non-Hispanic Black and those stratified in the lowest SES group, suggesting provider bias may impact the decision to make a referral. The decision to call CPS should occur independently of a patient’s race or SES level. In order to mitigate subjective decision-making, we propose the following objective CPS referral criteria to standardize the process in UI cases: patients requiring admission or medical intervention, ingestion of an illicit/controlled substance, prior ingestion, concern for safety or malicious intent, history inconsistent with developmental abilities, delay in seeking care, or if recommended by a child abuse physician.
.png)