Hospital Medicine: Hospital Medicine Quality Improvement
Hospital Medicine 1
741 - A Quality Improvement Initiative to Improve Discharge Communication for Children with Medical Complexity Through the Use of a Standardized Template
Friday, April 28, 2023
5:15 PM - 7:15 PM ET
Poster Number: 741
Publication Number: 741.119
Publication Number: 741.119
Yomna Farooqi, Icahn School of Medicine at Mount Sinai, Plano, TX, United States; Elaine Lin, Icahn School of Medicine at Mount Sinai, New York, NY, United States; Jasmine M. Blake, Icahn School of Medicine at Mount Sinai, New York, NY, United States; Matthew Deng, Mount Sinai Hospital, New York, NY, United States; Deanna Chieco, Mount Sinai School of Medicine, Mamaroneck, NY, United States; Laura N. Hodo, Icahn School of Medicine at Mount Sinai, Hastings on Hudson, NY, United States; Jan Fune, Icahn School of Medicine at Mount Sinai, New York, NY, United States
- EL
Elaine Lin, MD
Associate Professor of Pediatrics
Icahn School of Medicine at Mount Sinai
New York, New York, United States
Presenting Author(s)
Background: Children with Medical Complexity (CMC) have increased care coordination needs which places them at increased risk for poor discharge communication during care transitions. Poor discharge communication between the inpatient and outpatient medical providers can lead to decreased patient safety, lower clinician satisfaction, higher resource utilization, and preventable adverse events after discharge. To evaluate this problem at our institution we conducted a needs assessment and spoke with our complex care outpatient providers from the Pediatric Visiting Doctors and Complex Care Program (PVD clinic) and parents of CMC. We found that the transfer of important information on discharge documentation was inconsistent and incomplete at times.
Objective: Our SMART Aim was to increase the use of a novel Complex Care Discharge Summary (CCDS) template from 0% to 60% over 6 months.
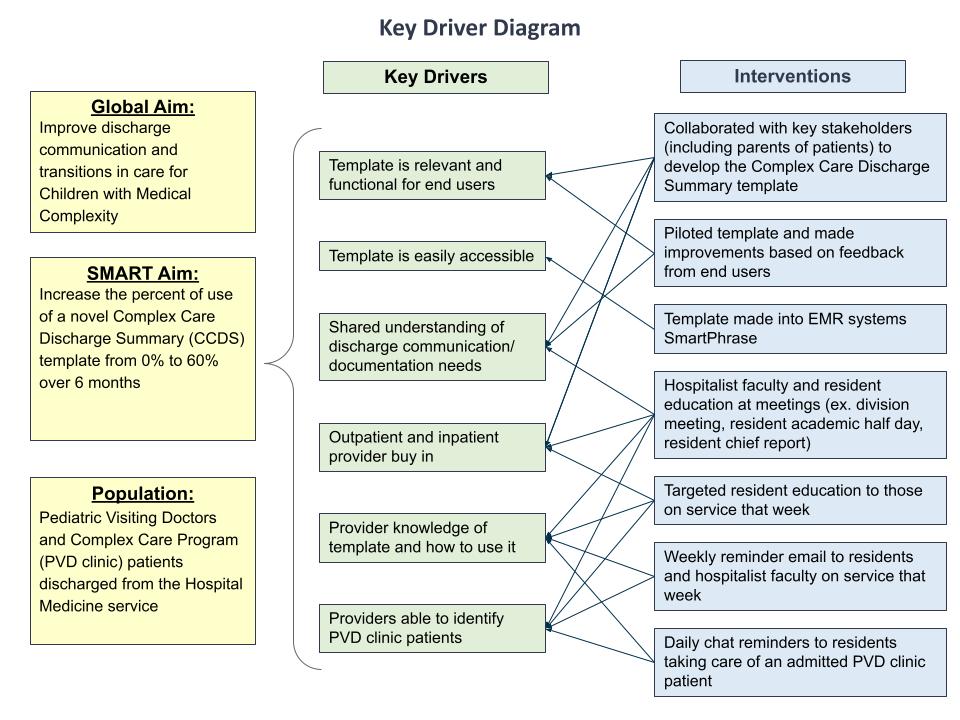
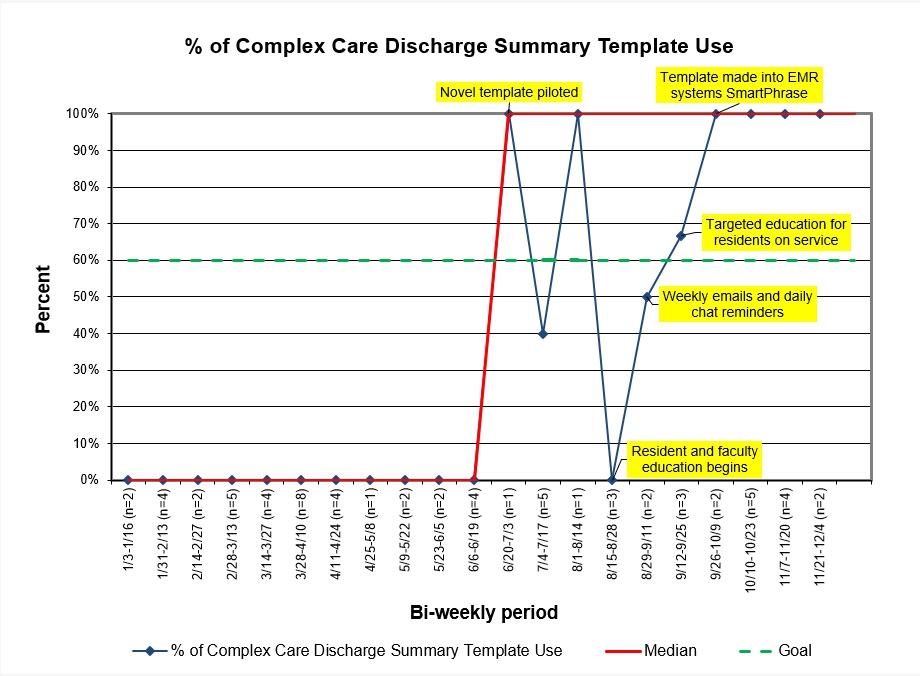
Design/Methods: We included patients enrolled in the PVD clinic who were discharged from the hospital medicine service at our institution. Our team worked together to build a novel CCDS template (Figure 3), create a process map, identify key drivers (Figure 1), and design Plan-Do-Study-Act (PDSA) cycles. Interventions included 1) piloting the template with end users to obtain feedback and make improvements, 2) resident and faculty education 3) weekly emails and daily Electronic Medical Record (EMR) chat reminders to the inpatient team, and 4) template made into an EMR systems SmartPhrase. Data were extracted from the EMR via a weekly report and manual chart review. Data were entered into an annotated run chart to track the effectiveness of our interventions over time.
Results: We reviewed 38 discharge summaries (DCS) during the baseline period and 28 DCS after implementing interventions. The median percentage of CCDS template use in eligible patients increased from 0% to 100% over 5 months (Figure 2).
Conclusion(s): We successfully implemented and increased the percentage of use of a novel Complex Care Discharge Summary template for CMC discharged from the hospital medicine service. Future PDSA cycles will target sustainability with reminder cards in resident team rooms and EHR-based interventions such as automatic template pull-in for CMC.
.jpg)
