Back
Background: Pediatricians are among the lowest-paid physicians. Despite additional training, for most pediatric subspecialists pursuing a subspecialty fellowship is a negative financial decision compared with practicing as a general pediatrician. Financial disadvantage by specialty in combination with high educational debt among trainees may shape the pediatric workforce.
Objective: Examine the association between self-reported educational debt and pediatric subspecialty fellowship type.
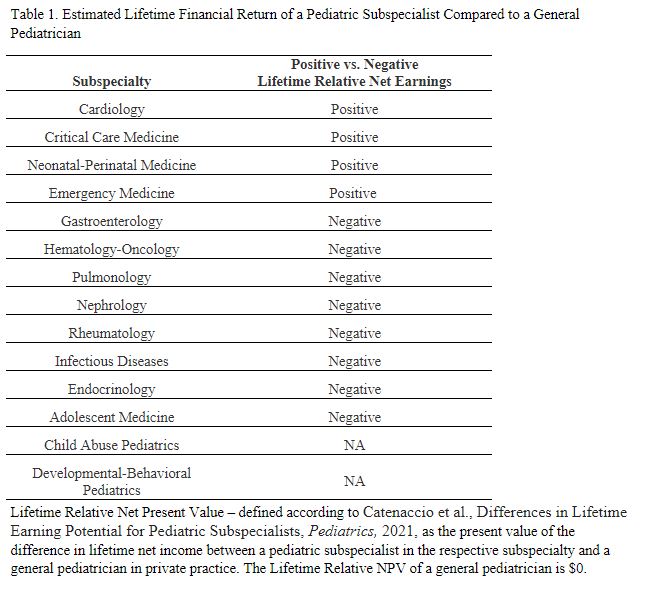
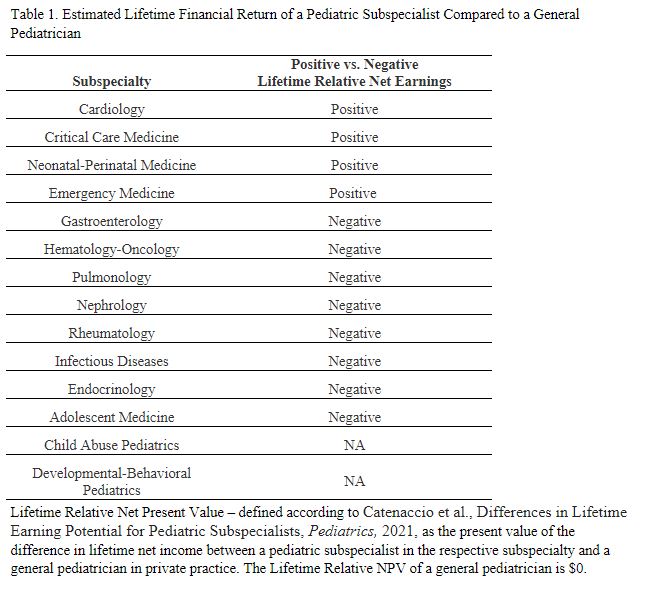
Design/Methods: Cross-sectional study of the American Board of Pediatrics Subspecialty In-training Examination (SITE) post-examination survey, administered annually to fellows enrolled in one of 14 subspecialties. The study sample consisted of first-year subspecialty fellows who completed the SITE survey during 2018, 2019, and 2021 (2020 data were excluded due to temporary changes in survey questions). The exposure of interest was self-reported educational debt. The outcome of interest was current subspecialty fellowship, dichotomized into positive and negative lifetime relative net present value subspecialties relative to a private practice general pediatrician (i.e., someone in a negative lifetime relative net present value subspecialty would earn less than a general pediatrician over their career) (Table 1). Ordinal logistic regression factor analysis models examined the association between debt and subspecialty type, adjusting for gender, region, International vs American medical graduate, and race/ethnicity.
Results: 3,264 pediatric fellows were included. In adjusted analysis, fellows with educational debt of $200,000 to < $300,000 had 1.39 aOR (95% CI 1.13-1.72) and those with >=$300,000 had 1.46 aOR (95% CI 1.19-1.79) of training in a positive lifetime relative net present value subspecialty (Table 2).
Conclusion(s): Understanding how pediatric resident’ educational debt influences subspecialty selection is an important, given 44% of pediatric interns report >$200,000 in educational debt. In this national study, educational debt was positively associated with training in a positive lifetime relative net present value subspecialty and may be an important contributor to workforce issues, such as shortages in smaller subspecialties. Diversification also could be exacerbated by residents with high debt preferentially choosing positive lifetime relative net present value subspecialties. Our findings may inform discussion around pediatric subspecialty workforce policy, including interventions addressing educational debt, such as loan repayment programs or free medical school tuition.
.jpg)
Medical Education: Fellow
Medical Education 3: Fellow 1
481 - : The Association Between Self-Reported Educational Debt and Subspecialty Type
Friday, April 28, 2023
5:15 PM – 7:15 PM ET
Poster Number: 481
Publication Number: 481.124
Publication Number: 481.124
Jennifer C. Gutierrez-Wu, UNC, Chapel Hill, NC, United States; Colin J. Orr, University of North Carolina at Chapel Hill School of Medicine, Chapel Hill, NC, United States; Victor Ritter, University of North Carolina at Chapel Hill School of Medicine, Redwood City, CA, United States; Adam Turner, The American Board of Pediatrics, 27617, NC, United States; Laurel K. Leslie, American Board of Pediatrics, Chapel Hill, NC, United States

Jennifer C. Gutierrez-Wu, MD (she/her/hers)
Primary Care Research Fellow
UNC
Chapel Hill, North Carolina, United States
Presenting Author(s)
Background: Pediatricians are among the lowest-paid physicians. Despite additional training, for most pediatric subspecialists pursuing a subspecialty fellowship is a negative financial decision compared with practicing as a general pediatrician. Financial disadvantage by specialty in combination with high educational debt among trainees may shape the pediatric workforce.
Objective: Examine the association between self-reported educational debt and pediatric subspecialty fellowship type.
Design/Methods: Cross-sectional study of the American Board of Pediatrics Subspecialty In-training Examination (SITE) post-examination survey, administered annually to fellows enrolled in one of 14 subspecialties. The study sample consisted of first-year subspecialty fellows who completed the SITE survey during 2018, 2019, and 2021 (2020 data were excluded due to temporary changes in survey questions). The exposure of interest was self-reported educational debt. The outcome of interest was current subspecialty fellowship, dichotomized into positive and negative lifetime relative net present value subspecialties relative to a private practice general pediatrician (i.e., someone in a negative lifetime relative net present value subspecialty would earn less than a general pediatrician over their career) (Table 1). Ordinal logistic regression factor analysis models examined the association between debt and subspecialty type, adjusting for gender, region, International vs American medical graduate, and race/ethnicity.
Results: 3,264 pediatric fellows were included. In adjusted analysis, fellows with educational debt of $200,000 to < $300,000 had 1.39 aOR (95% CI 1.13-1.72) and those with >=$300,000 had 1.46 aOR (95% CI 1.19-1.79) of training in a positive lifetime relative net present value subspecialty (Table 2).
Conclusion(s): Understanding how pediatric resident’ educational debt influences subspecialty selection is an important, given 44% of pediatric interns report >$200,000 in educational debt. In this national study, educational debt was positively associated with training in a positive lifetime relative net present value subspecialty and may be an important contributor to workforce issues, such as shortages in smaller subspecialties. Diversification also could be exacerbated by residents with high debt preferentially choosing positive lifetime relative net present value subspecialties. Our findings may inform discussion around pediatric subspecialty workforce policy, including interventions addressing educational debt, such as loan repayment programs or free medical school tuition.
.jpg)
