Back
Background: Despite their effects on children’s health, race and racism are not routinely discussed during pediatric outpatient visits. Whether families want to discuss race and racism with their pediatrician and how to do so effectively has not been previously studied.
Objective: We sought to explore family members’, community members’ and pediatric residents’ perspectives on discussing race and racism during outpatient pediatric visits.
Design/Methods: We recruited pediatric residents training at a large urban academic pediatric quaternary care center, physician parents, and non-physician community members by inviting them to participate in focus groups via email. Participants were recruited to ensure diverse racial representation and divided into focus groups based on their self-identified race. We used semi-structured interview guides to facilitate focus group discussions with each participant group, which were led by race-concordant facilitators. We recorded and transcribed the focus group dialogue and used constant comparison to generate codes and determine relationships between and within codes to generate themes.
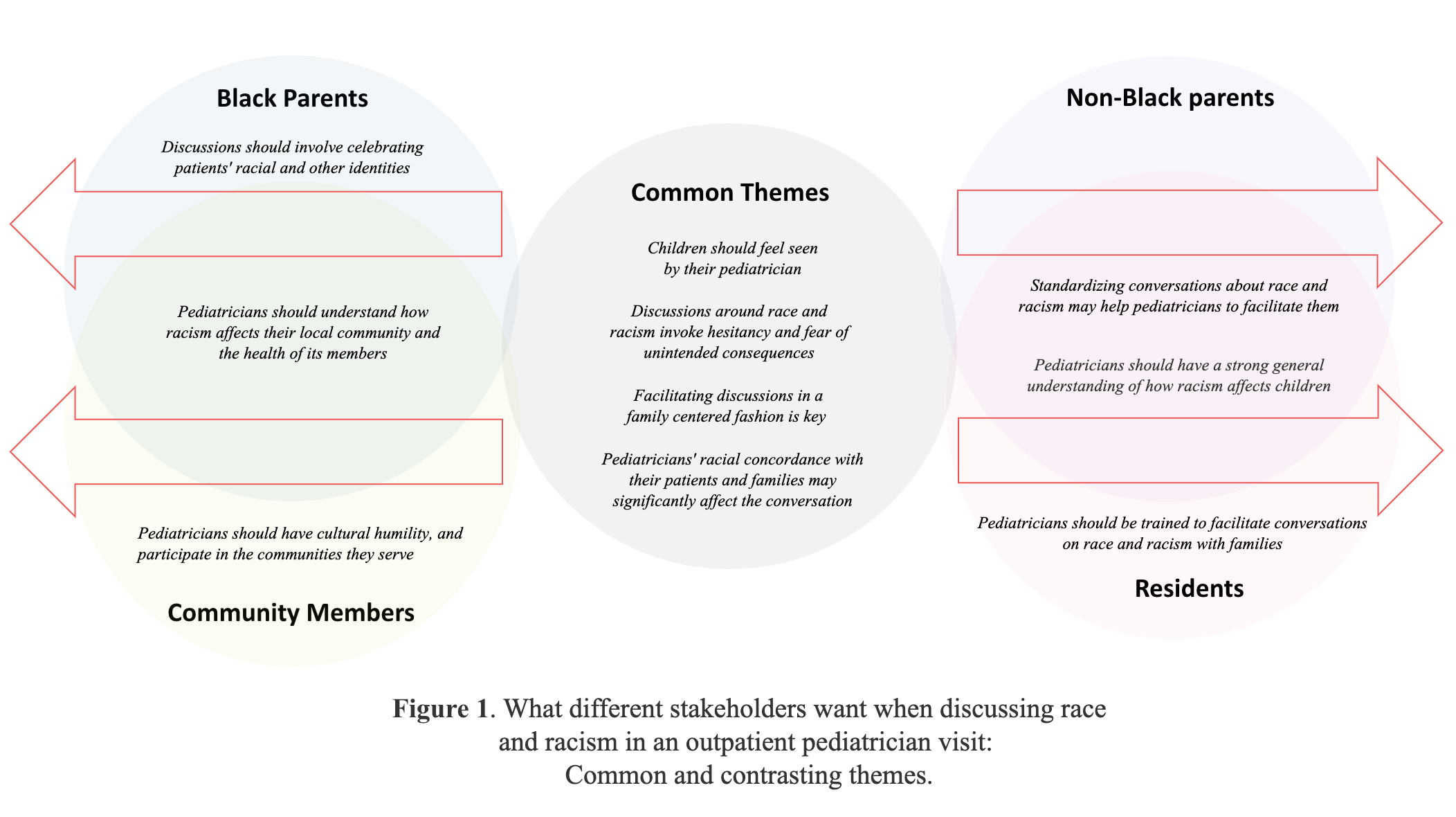
Results: We facilitated 5 focus groups with 15 total participants. We identified 10 themes, including 4 common themes across participant groups and 6 contrasting themes shared by some groups (Figures 1-3). All groups wanted to discuss race in a family-centered way and for children to feel seen by their pediatrician. All groups also expressed hesitancy in discussing racism due to fear of unintended consequences and expressed that provider-family racial concordance may help to facilitate these discussions. Black parents wanted their pediatrician to celebrate their children’s racial and other identities. Community members discussed the importance of pediatricians belonging to their communities and showing cultural humility. Both Black parents and community members wanted their pediatrician to understand how racism affects their local community. Residents felt pediatricians should be trained to facilitate race-based discussions. Both non-Black parents and residents felt that understanding racism’s effects on children is important and standardizing conversations may help with facilitation.
Conclusion(s): Discussions about race and racism should be facilitated in an individualized, family-centered manner that allows children to feel seen, and adverse consequences should be considered. Needs amongst stakeholder groups vary, and sometimes conflict, regarding how to best facilitate these discussions in the pediatric primary care setting.
.png)
.png)
Medical Education: Diversity, Equity & Inclusion
Medical Education 4: Diversity, Equity, & Inclusion 1
506 - Talking about Race and Racism in the Primary Care Setting: Common and Conflicting Needs for Families, Learners, and Community Members
Friday, April 28, 2023
5:15 PM – 7:15 PM ET
Poster Number: 506
Publication Number: 506.125
Publication Number: 506.125
Josh Kurtz, Childrens Hospital of Philadelphia, Philadelphia, PA, United States; Emma Hackel, Childrens Hospital of Philadelphia, Philadelphia, PA, United States; Sophie Lieberman, Childrens Hospital of Philadelphia, Philadelphia, PA, United States; Christine Cummings, Childrens Hospital of Philadelphia, Philadelphia, PA, United States; Hannah Anderson, Children's Hospital of Philadelphia, Philadelphia, PA, United States; Aditi Vasan, Children's Hospital of Philadelphia, Philadelphia, PA, United States; Noreena S. Lewis, Children's Hospital of Philadelphia, Wilmington, DE, United States; George Dalembert, Childrens Hospital of Philadelphia, Philadelphia, PA, United States; Jessica Fowler, Perelman School of Medicine at the University of Pennsylvania, Philadelphia, PA, United States; Beth Rezet, Childrens Hospital of Philadelphia, Havertown, PA, United States

Josh Kurtz, MD (he/him/his)
Pediatric resident, PGY-3
Childrens Hospital of Philadelphia
Philadelphia, Pennsylvania, United States
Presenting Author(s)
Background: Despite their effects on children’s health, race and racism are not routinely discussed during pediatric outpatient visits. Whether families want to discuss race and racism with their pediatrician and how to do so effectively has not been previously studied.
Objective: We sought to explore family members’, community members’ and pediatric residents’ perspectives on discussing race and racism during outpatient pediatric visits.
Design/Methods: We recruited pediatric residents training at a large urban academic pediatric quaternary care center, physician parents, and non-physician community members by inviting them to participate in focus groups via email. Participants were recruited to ensure diverse racial representation and divided into focus groups based on their self-identified race. We used semi-structured interview guides to facilitate focus group discussions with each participant group, which were led by race-concordant facilitators. We recorded and transcribed the focus group dialogue and used constant comparison to generate codes and determine relationships between and within codes to generate themes.
Results: We facilitated 5 focus groups with 15 total participants. We identified 10 themes, including 4 common themes across participant groups and 6 contrasting themes shared by some groups (Figures 1-3). All groups wanted to discuss race in a family-centered way and for children to feel seen by their pediatrician. All groups also expressed hesitancy in discussing racism due to fear of unintended consequences and expressed that provider-family racial concordance may help to facilitate these discussions. Black parents wanted their pediatrician to celebrate their children’s racial and other identities. Community members discussed the importance of pediatricians belonging to their communities and showing cultural humility. Both Black parents and community members wanted their pediatrician to understand how racism affects their local community. Residents felt pediatricians should be trained to facilitate race-based discussions. Both non-Black parents and residents felt that understanding racism’s effects on children is important and standardizing conversations may help with facilitation.
Conclusion(s): Discussions about race and racism should be facilitated in an individualized, family-centered manner that allows children to feel seen, and adverse consequences should be considered. Needs amongst stakeholder groups vary, and sometimes conflict, regarding how to best facilitate these discussions in the pediatric primary care setting.
.png)
.png)

