Endocrinology: Transgender
Endocrinology 1
191 - Gender Affirming Medical Treatment and It's Impact on ED utilization in a large Safety net system
Publication Number: 191.213

Margaret M. Tomcho, MD (she/her/hers)
Medical Director for Pre-Health Programs
Denver Health
Denver, Colorado, United States
Presenting Author(s)
Background: There is a well-documented mental health crisis among youth. The literature suggests that this crisis has led to increased emergency department (ED) utilization which can be traumatic and exacerbate mental health issues. Youth who identify as transgender (TG) have higher rates of mental health (MH) issues compared to cis-gender peers including depression, self-harm and suicidal ideation (SI). These MH issues can result in increased ED utilization.
Objective:
To examine the impact of medical interventions such as puberty blockers and/or gender affirming hormones (GAH) for TG youth on ED utilization.
Design/Methods:
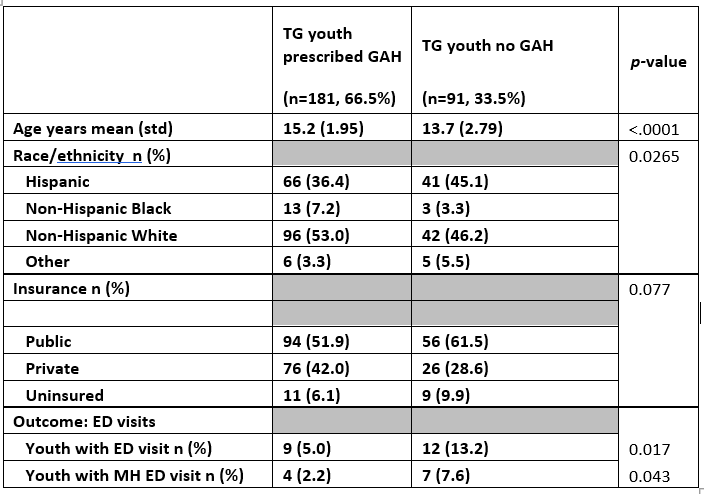
Denver Health and Hospitals (DHH) is an integrated system of Federally Qualified Health Centers (FQHCs) providing care for under-resourced communities in Denver and surrounding region. Since 2016, a group of pediatricians were trained as champions to provide gender affirming care including puberty blockers and GAHs within the primary care medical home. The goals were to increase continuity within the medical home and decrease barriers for these youth. Youth 18 years and under with a diagnosis of gender dysphoria (GD) currently being treated with puberty blockers or GAH were compared with those not receiving medical intervention. Outcomes of department (ED) utilization were compared dichotomously by rates of one-year utilization. Data were collected by retrospective EMR review of youth seen in 2019-2021.
Results: Youth not provided medical intervention for GD were significantly more likely to have an ED visit within one year for mental health issues (p=0.043) or for any reason, including medical issues (p=0.017). Mental health diagnoses included depression (n=5), SI (2) mood disorders (2), anxiety (1), and self-harm (1). There were no significant differences between groups in race/ethnicity (p=0.265) or payer (p=.077). Age was significantly different between groups (p< .001). Logistic regression confirms the association between ED visits within one year and GAH treatment when adjusting for age (p = .015).
Conclusion(s):
TG youth prescribed either puberty blockers or GAH had less ED utilization for mental health issues and overall. Data on whether youth without medical interventions had wanted this care is not available but would be important to assess, as this could be related to age. Increasing access to gender affirming care for publicly insured and uninsured youth remains a high priority. Providing gender affirming care to youth is critical for preventing serious mental health outcomes, especially suicide and for overall promotion of health and well-being.