Neonatal General
Neonatal General 6: Neurology
718 - A paradigm shift in judging the risk of intraventricular hemorrhage in relation to intravenous fluid bolus in extremely premature newborns within seventy-two hours of birth.
Saturday, April 29, 2023
3:30 PM - 6:00 PM ET
Poster Number: 718
Publication Number: 718.234
Publication Number: 718.234
Aashika Janwadkar, John H. Stroger Hospital of Cook County, Chicago, IL, United States; Bilal Manzoor, John H Stroger, Jr. Hospital of Cook County, Chicago, IL, United States; Ebuwa Joy Obaseki, John H. Stroger, Jr Hospital of Cook County, Chicago, IL, United States; Dhaivat Shah, Ann & Robert H. Lurie Children's Hospital of Chicago, Chicago, IL, United States; Christian Castillo, Cook Children's Medical Center, chicago, IL, United States

Aashika Janwadkar, MD (she/her/hers)
Fellow
John H. Stroger Hospital of Cook County
Chicago, Illinois, United States
Presenting Author(s)
Background: Various predictors associated with development of severe intraventricular hemorrhage (IVH) have been identified in literature such as failure to receive antenatal steroids, male sex, 5 min Apgar score < 7, intubation at birth, extremely low gestational age, transfer from other NICU (Neonatal Intensive Care Unit) and vaginal delivery. There is a paucity of evidence on the impact of intravenous (IV) boluses as a risk factor for IVH in extremely premature neonates.
Objective: To investigate the association of IV bolus given within 72 hours of birth to premature neonates between 22 weeks to 28 weeks of gestation with the risk of development of IVH.
Design/Methods: A retrospective cohort study done in a tertiary-level neonatal intensive care unit from January 2017 to December 2022. The infants included in this study were extremely premature neonates between 22 weeks to 28 weeks of gestation, who received at least one 10 ml/kg of IV normal saline bolus within 72 hours of birth and had a head ultrasound within 7 days of birth. Classification of IVH used as per J. Volpe. SAS 9.4 version was used for statistical analysis. Univariable analysis of categorical variables performed with the chi-square test or fisher’s exact test, and for continuous variables done with student’s t-test. Multivariable logistic regression analysis was done to identify the predictors of IVH.
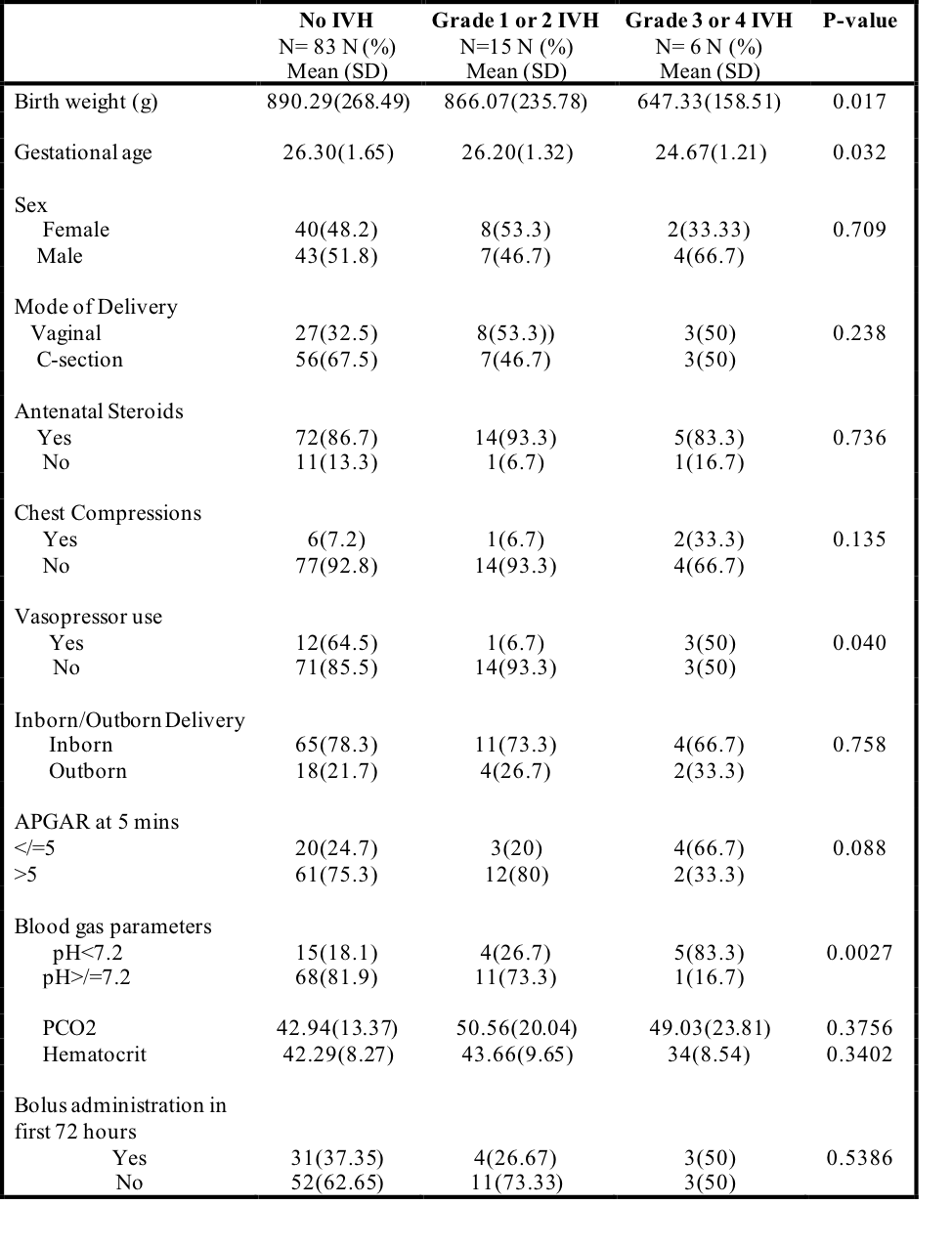
Results: 104 infants were included in this study. Birthweight, gestational age, vasopressors use in first 72 hours of life and pH were significant (p=0.017, p=0.032, p=0.040, p=0.0027 respectively) (Table 1). Fluid bolus was not significant on univariable analysis (OR 1.8, 95%CI 0.345-9.399, p=0.486); however, pH was significant (OR 20.78, 95% CI 2.293-188.435, p= 0.007). On multivariable logistic regression patients with pH value < 7.2, had 16.6 times the Odds of grade 3 or 4 IVH compared to the patients with pH value >=7.2 (aOR=16.63, 95%CI=1.46 - 189.01, p:0.02) after adjusting for baseline variables. IV bolus on multivariable logistic regression was not significant (aOR=0.46, 95%CI=0.061-3.555, p=0.46).
Conclusion(s): This study reveals IV fluid bolus administration to extremely premature neonates within 72 hours of birth is not associated with increased risk of IVH, but caution should be exercised when interpreting the results as the sample size for higher grades of IVH was small and further large multicenter studies are needed to find the association between IV bolus and risk of development of IVH.
.png)
