Neonatal Nephrology/AKI
Neonatal Nephrology/AKI 2
242 - Early Fluid Status and Prediction of Severe Intraventricular Hemorrhage or Death in Extremely Preterm Infants
Saturday, April 29, 2023
3:30 PM - 6:00 PM ET
Poster Number: 242
Publication Number: 242.243
Publication Number: 242.243
Lucinda Weaver, University of Alabama at Birm, BIRMINGHAM, AL, United States; Samuel Gentle, University of Alabama at Birmingham, Birmingham, AL, United States; Vivek Shukla, University of Alabama at Birmingham, Birmingham, AL, United States; Arie Nakhmani, University of Alabama at Birmingham, Birmingham, AL, United States; AKM F. Rahman, University of Alabama at Birmingham, Birmingham, AL, United States; Namasivayam Ambalavanan, University of Alabama School of Medicine, Birmingham, AL, United States; David Askenazi, University of Alabama at Birmingham, BIRMINGHAM, AL, United States; Colm P. Travers, University of Alabama School of Medicine, Birmingham, AL, United States

Lucinda Weaver, MD
Fellow PGY VI
University of Alabama at Birm
BIRMINGHAM, Alabama, United States
Presenting Author(s)
Background: Extremely preterm infants are at high risk of severe intraventricular hemorrhage (IVH) and death. Postnatal weight loss due to natriuresis and diuresis is part of extrauterine adaptation. Fluid and sodium management influence this process and are associated with IVH.
Objective: The purpose was to determine measures of fluid balance that predict severe IVH or death in the first postnatal week.
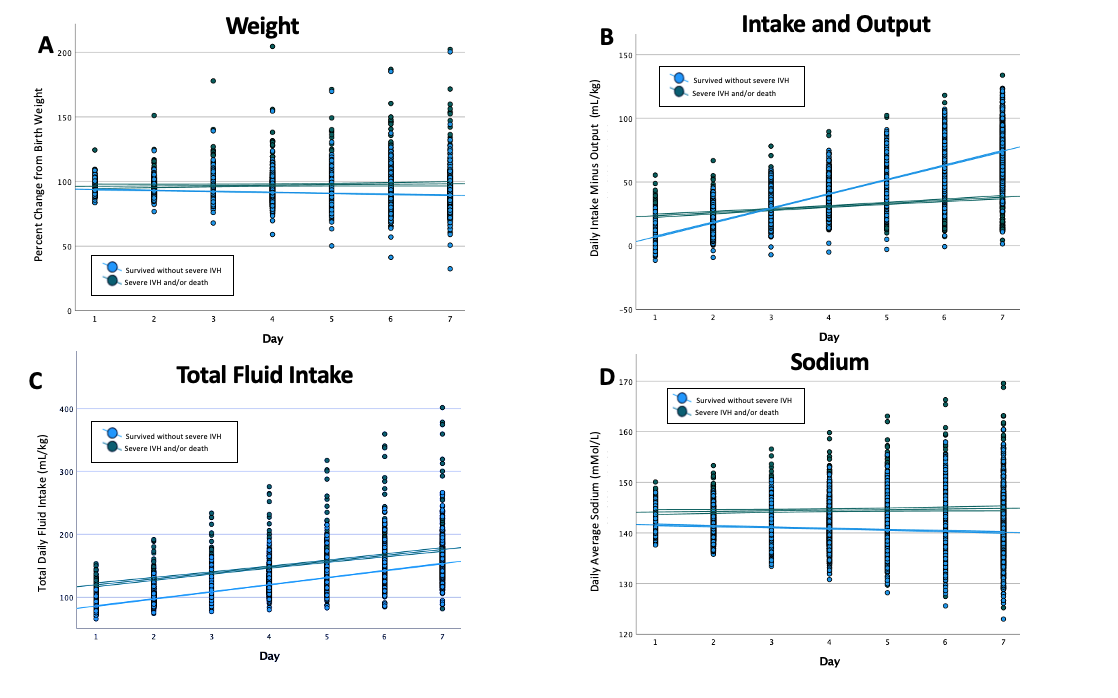
Design/Methods: Single-center, retrospective cohort analysis included actively treated inborn infants with birth weight (BW) ≥400 grams and gestational ages (GA) from 220/7 to 276/7 weeks at the University of Alabama at Birmingham from 2014-2021. Infants with major congenital anomalies were excluded. Daily data was collected including sodium, percent weight change from BW, total parenteral fluid intake and urine output, and fluid balance (total input-output) during the first postnatal week. Longitudinal mixed effect models compared fluid balance covariates throughout the first postnatal week among infants with and without severe IVH or death (figure 1). Multivariable logistic regression and machine learning (ML) models using ensemble RUS boosted decision trees were developed with and without adjusting for baseline characteristics, including GA, BW, antenatal steroids, multiples, and sex to assess the prediction accuracy for severe IVH or death using area under the receiver operating curves (AUC).
Results: The mean gestation of infants included (n=932) was 25w2d ± 1w4d, and the average birth weight (BW) of 746±212 grams (g). Infants with severe IVH or death (n=195) had a lower GA (24w±1.6 vs. 26w±1.4; p< 0.001) and BW (621±176g vs. 779±209g) than infants who survived without severe IVH (n=737). Lower percent change from BW (p< 0.001), higher total fluid intake (p=0.007), higher Na (p=0.007), and a relatively equal fluid balance (p< 0.001) [Figure 1] were associated with severe IVH and/or death in the first postnatal week after adjustment for baseline characteristics. Daily urine output did not differ significantly between groups (p=0.08). The AUC for regression models predicting IVH and/or death incorporating baseline characteristics improved by adding fluid balance measures from 0.70 to 0.79. The AUC for ML-models using baseline characteristics improved from 0.72 (accuracy (ACC) - 68.3%) to 0.83 (ACC - 83%) with the addition of fluid balance measures.
Conclusion(s): In extremely preterm infants, measures of early fluid balance improve the prediction of severe IVH and/or death compared with models incorporating baseline characteristics alone.