General Pediatrics: Primary Care/Prevention
General Pediatrics 4
476 - Pediatric Providers Current Practices and Comfort with Palliative Care Services in the Outpatient Setting: A Needs Assessment
Publication Number: 476.217

Casey Mason, Resident (she/her/hers)
Pediatric Resident
NY-Presbyterian
NEW YORK, New York, United States
Presenting Author(s)
Background:
Pediatric Palliative Care (PPC) provides integrated care addressing quality of life for children with complex or terminal illnesses including symptom management, social/emotional support, and advanced care planning. The establishment of outpatient palliative care has been shown to improve overall symptom control and quality of life. Primary care pediatricians (PCP) have an opportunity to build capacity using palliative care principles based on existing relationships and established practices of addressing psychosocial and emotional needs of patients.
Objective:
To assess the current practices and comfort by pediatric outpatient providers in providing palliative care services for patients in the primary care setting.
Design/Methods:
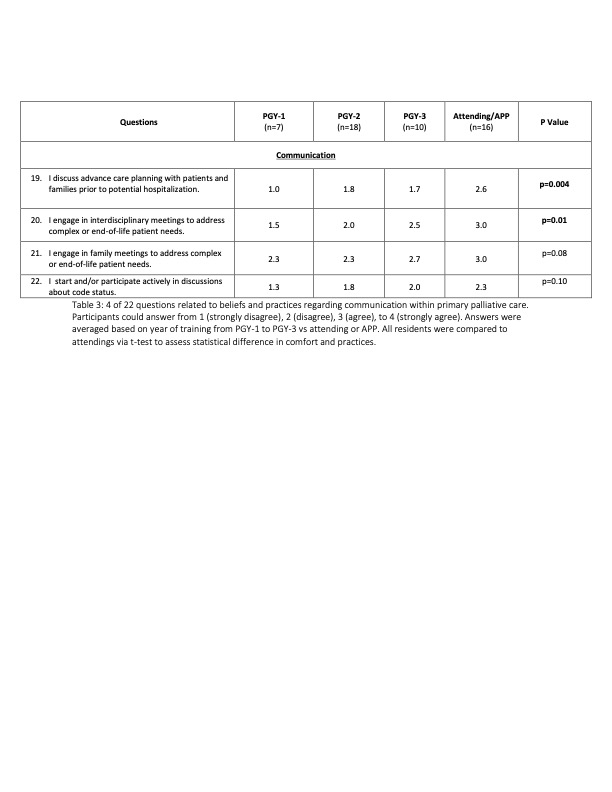
This study employed a quantitative survey of outpatient providers including residents, attendings, and advanced practice providers (APP) in the ambulatory care network of a large academic center. The survey was adapted from the End-of-Life Professional caregiver survey, a validated survey addressing the 8 domains of the national palliative care guidelines. The survey was reviewed by complex care and PPC content experts to establish content validity and consisted of 22 questions using a 4-point Likert scale (1-strongly disagree to 4-strongly agree). The survey was administered anonymously via Qualtrics to all eligible participants. Resident responses across all three years were compared to attending/APP responses using a two sample t-test.
Results: A total of 56 providers out of 105 participants recruited (28 faculty, 77 residents) responded (response rate 53%). While most providers felt comfortable identifying patients who may benefit from end-of-life care, providers across training levels disagreed/strongly disagreed with most statements regarding comfort in effective care delivery (Table 1), cultural and ethical considerations (Table 2), and communication (Table 3) for patients at the end-of-life care in the outpatient setting. Comparing attendings to residents revealed statistically significant difference most notably in the domains of communication and cultural and ethical considerations. Interestingly, attendings were more likely to defer/refer to subspecialists than residents despite more comfort in providing PPC services.
Conclusion(s):
PCPs are in a unique position to address the need for PPC services in the outpatient setting. This study showed clear need for future interventions to address primary care providers comfort level and current behaviors regarding primary palliative care practices that best align with national palliative care guidelines.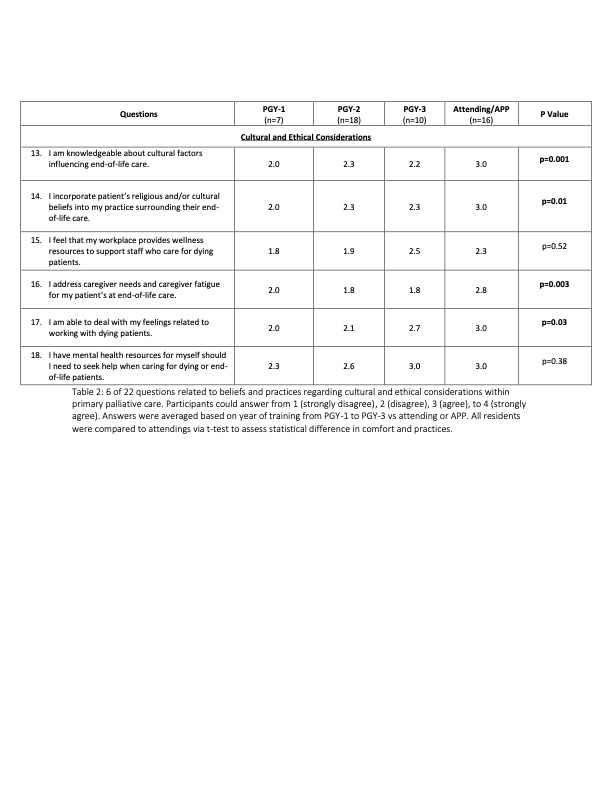
.png)
