Health Services Research
HSR 2: Clinical Explorations, Associations, and Interventions
591 - Preparing Fathers to Take a Leading Role in Preterm Birth
Publication Number: 591.223
- SM
Siobhan McDonnell, MS (she/her/hers)
Clinical Research Assistant
Medical College of Wisconsin
Wauwatosa, Wisconsin, United States
Presenting Author(s)
Background:
Fathers’ involvement in pregnancy is linked to better health outcomes, including fewer preterm births. For pregnancies at risk for preterm birth, barriers to receiving anticipatory education are greater for fathers. We created the smartphone Preemie Prep for Parents (P3) program to deliver information recommended to prepare parents for a preterm birth.
Objective: Examine the effect of the P3 program on fathers’ preterm birth knowledge and their preparation to participate in healthcare decisions impacting the preterm infant.
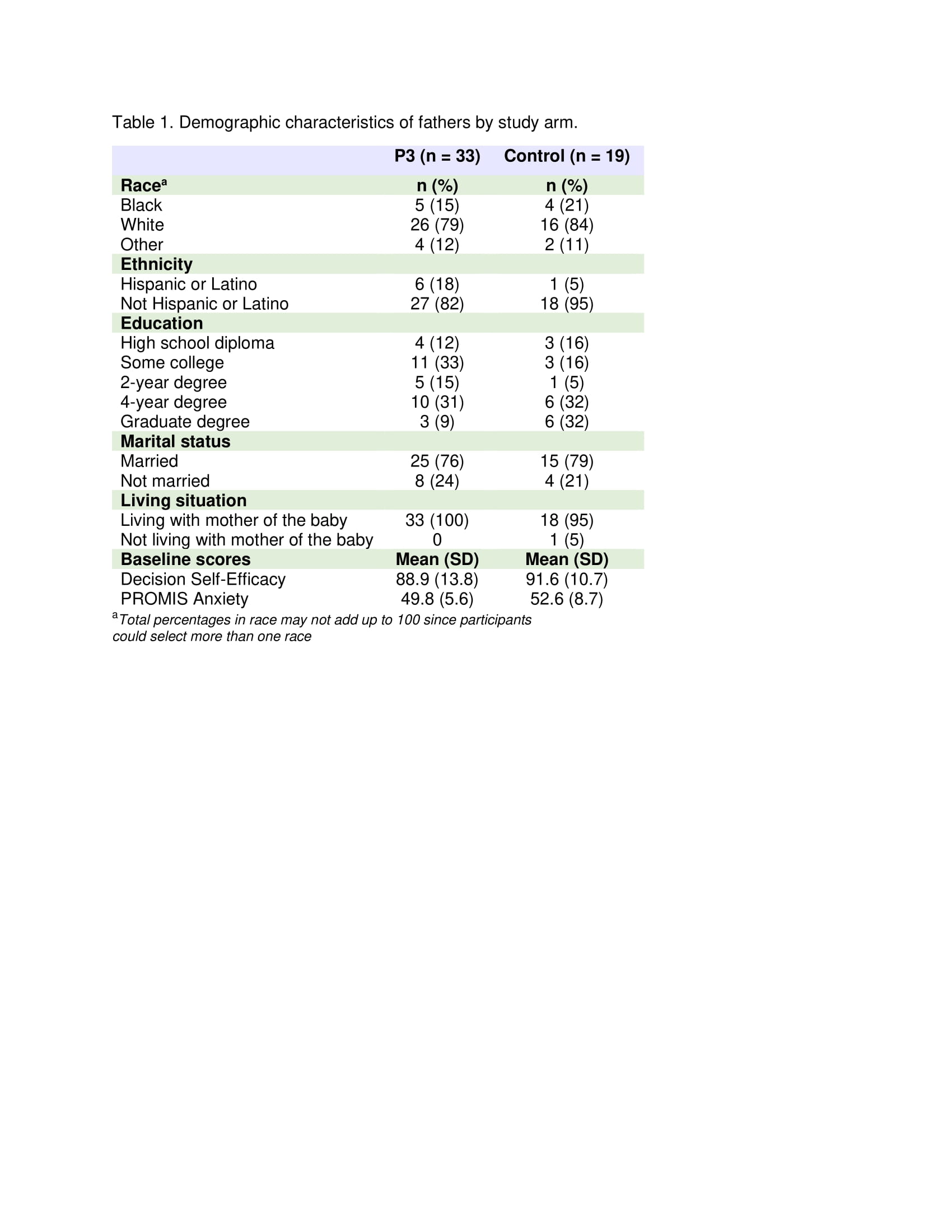
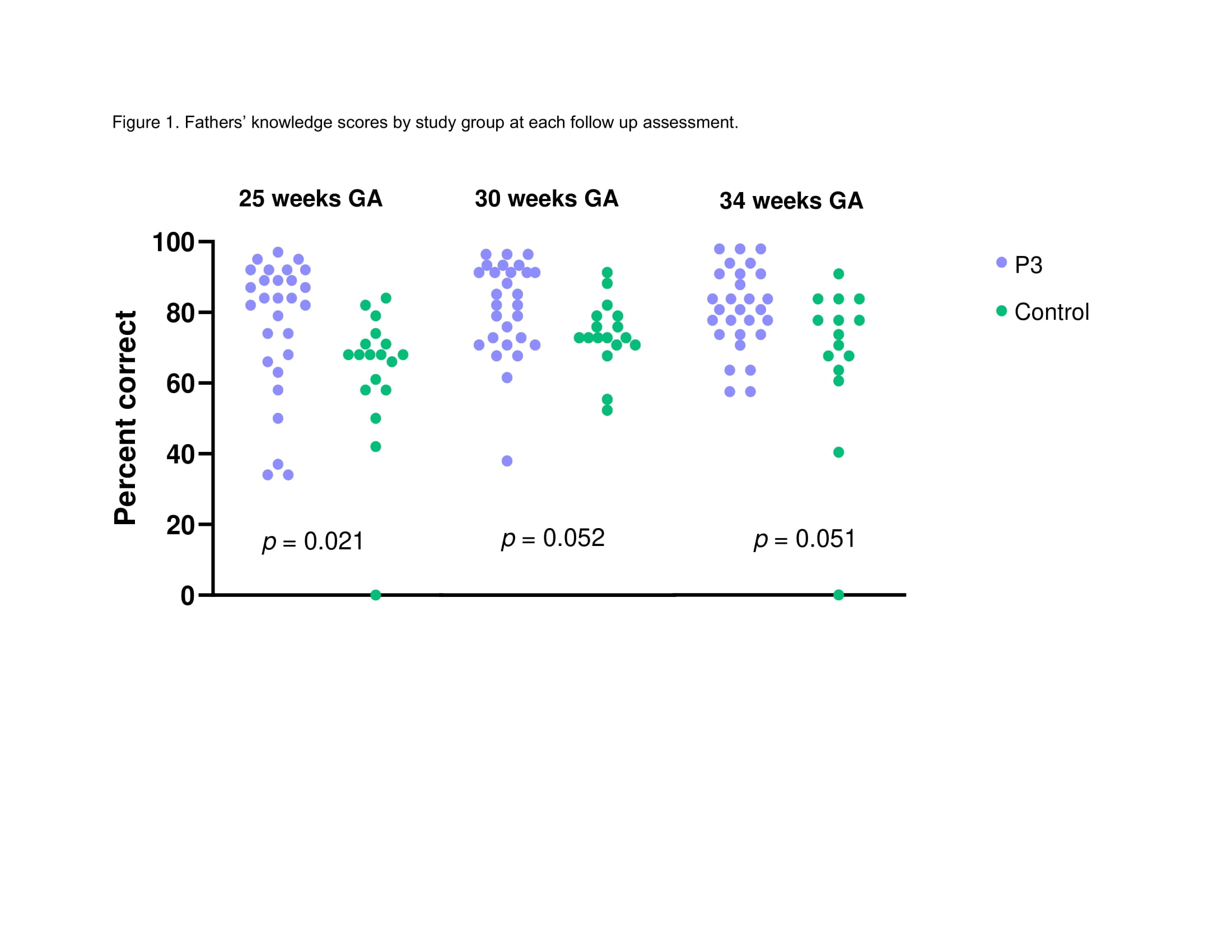
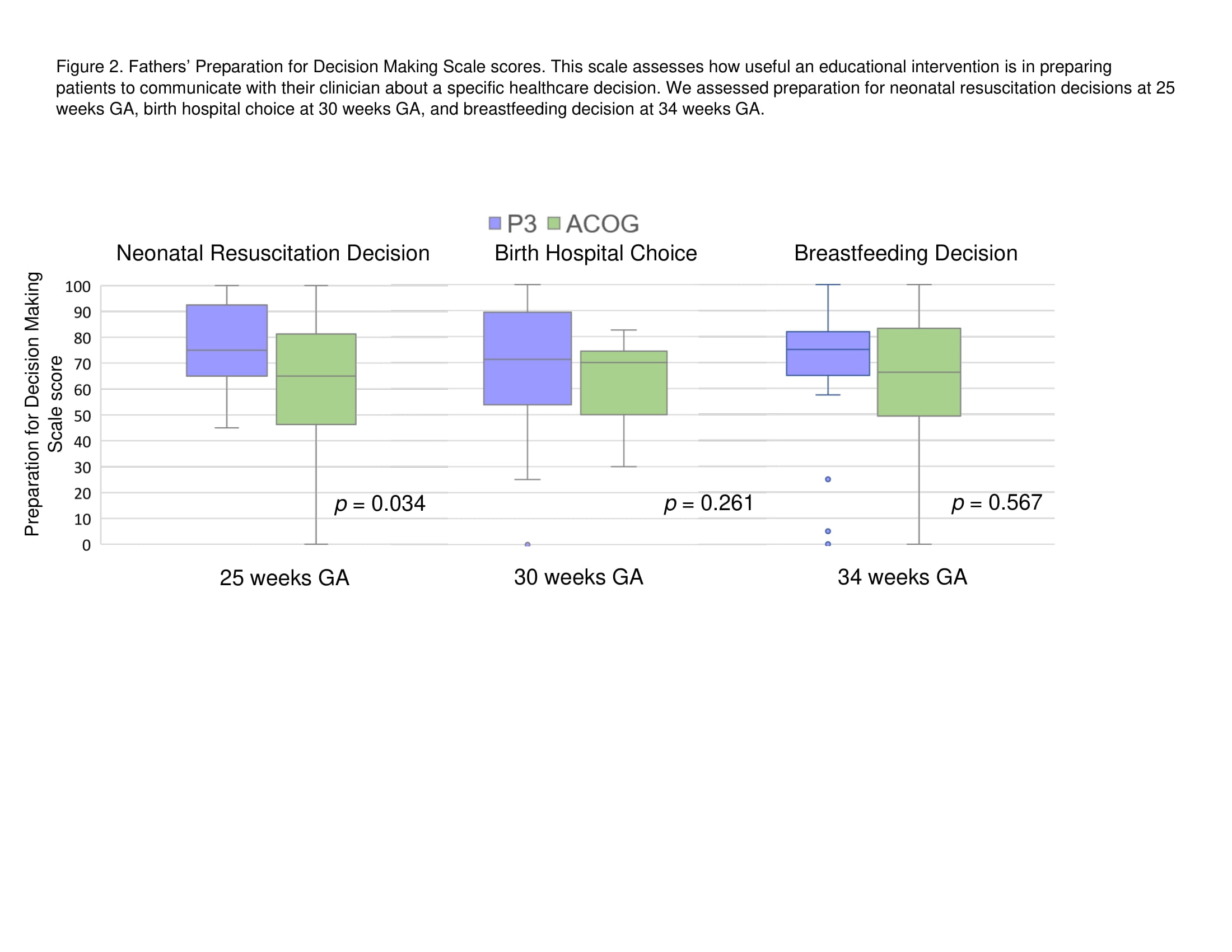
Design/Methods: This is an ancillary analysis of the fathers who participated in a randomized controlled trial (NCT04093492). Parents in the P3 arm received periodic text messages, starting as early as 18 weeks gestational age (GA) and until 34 weeks GA if pregnancy continued. Each P3 text message had a link to 1 of 51 short, animated, GA-specific videos. Parents in the control arm received links at enrollment to American College of Obstetricians and Gynecologists patient webpages. If the father of the baby participated, the mother-father pair were randomized together to prevent contamination. At enrollment, responses to PROMIS Anxiety and the Decision Self-Efficacy Scale were collected. If pregnancy continued, at 25, 30, and 34 weeks GA, responses to the Prematurity Knowledge Questionnaire, Preparation for Decision Making Scale, and PROMIS Anxiety were collected. P3 software tracked video use.
Results:
Of the 120 mothers, 52 (43%) participated with the baby’s father (Table 1). Fathers’ anxiety did not increase over time (Ps > 0.30) and did not differ between study arms (Ps > 0.09). On average, fathers in the P3 arm watched 41% of the 51 videos. Preterm birth knowledge scores were higher for fathers in the P3 arm (n=33) than the control arm (n=19) at 25 weeks GA, but the difference did not reach significance at 30 and 34 weeks GA (Figure 1). Fathers in the P3 arm were more prepared than in control arm to participate in neonatal resuscitation decisions at 25 weeks GA; however, the difference did not reach significance at 30 weeks GA focusing on birth hospital choice or 34 weeks GA focusing on breastfeeding decision (Figure 2).
Conclusion(s): The P3 program increases fathers’ knowledge without increasing their anxiety and prepares them for resuscitation decision making. An adequately powered study is needed to assess the full impact of the P3 program on fathers preparing for preterm birth. The P3 program may be beneficial for families with high-risk pregnancies.