Emergency Medicine: All Areas
Emergency Medicine 6
349 - Association of Self-Reported Suicide Risk Factors with Mental Health Return Visits in a Pediatric Emergency Department
Publication Number: 349.21
.jpg)
Rachel Cafferty, MD (she/her/hers)
Assistant Professor
University of Colorado School of Medicine
Aurora, Colorado, United States
Presenting Author(s)
Background:
Suicide is a leading cause of death for children in the United States. Routine screening for suicidal ideation (SI) and risk factors associated with a future suicide attempt allows for earlier detection of risk and intervention prior to crisis. Little is known about the association between self-reported risk factors and subsequent Emergency Department (ED) utilization for mental or behavioral health concerns.
Objective:
Characterize self-reported risk profiles among youth presenting to the ED and determine the association between risk factors and ED mental health return visits.
Design/Methods: Youth aged 10 to 18 years, presenting to the ED between July 2020 and May 2022, underwent routine suicide screening with the validated Ask Suicide Screening Questions (ASQ). Youth with a ‘positive’ screen were asked to complete a secondary survey of known risk factors associated with suicide. ED return rate for mental health concerns was determined at 6 months after the index visit. This was a retrospective cohort study. Risk profiles between patients with an ED mental health return visit were compared to those without a return visit using chi-square and Fisher’s exact tests. The association between an ED mental health return visit and risk factors, chosen a priori, were examined with multivariable logistic regression.
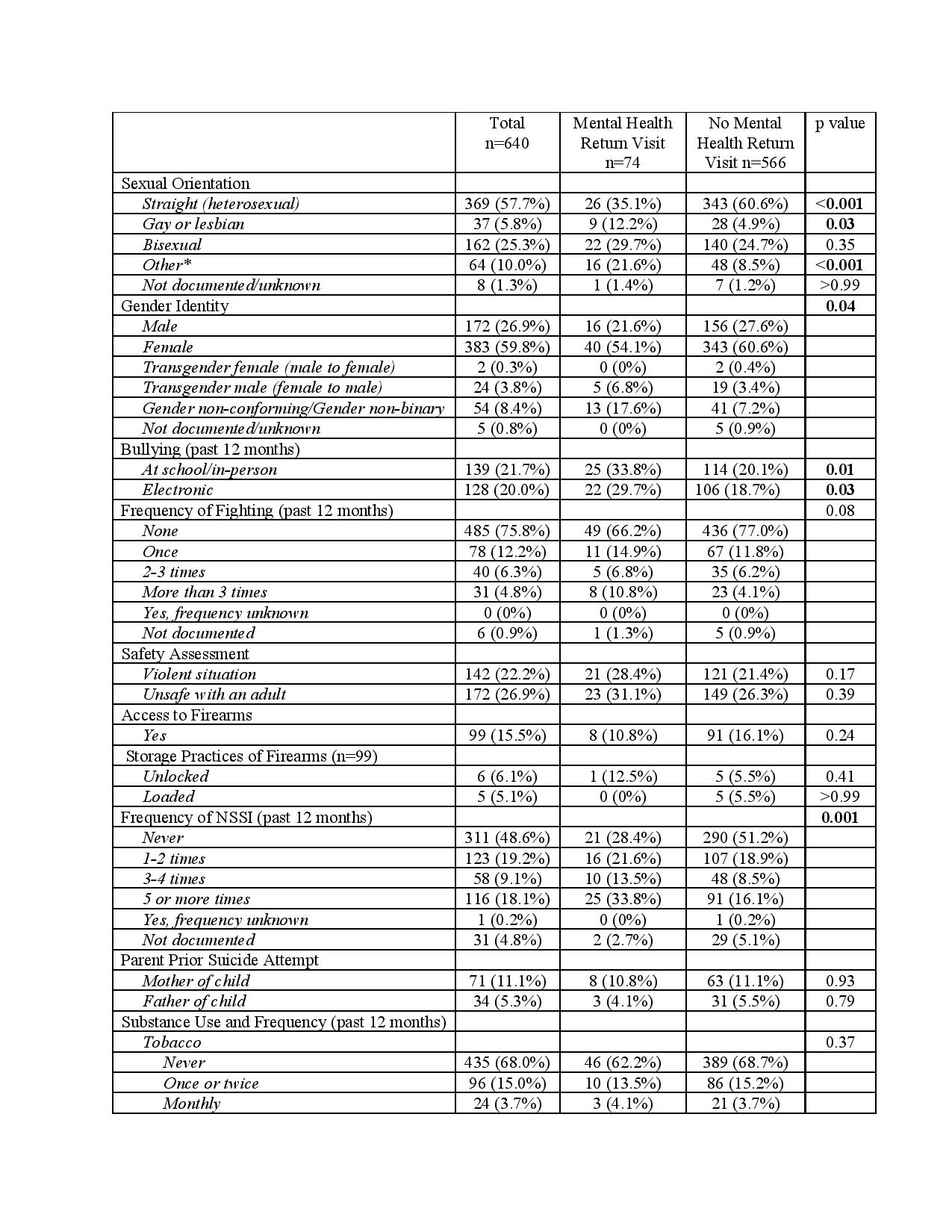
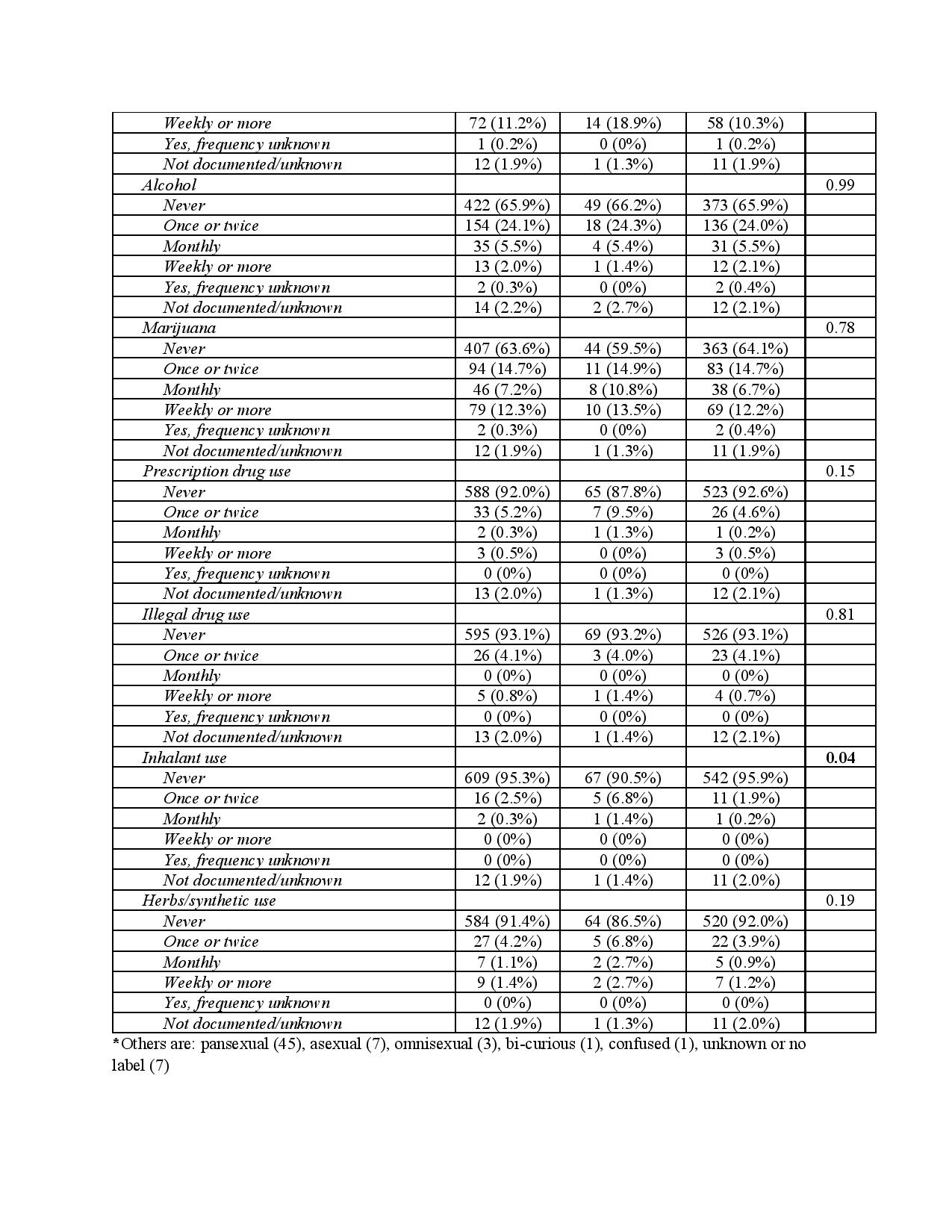
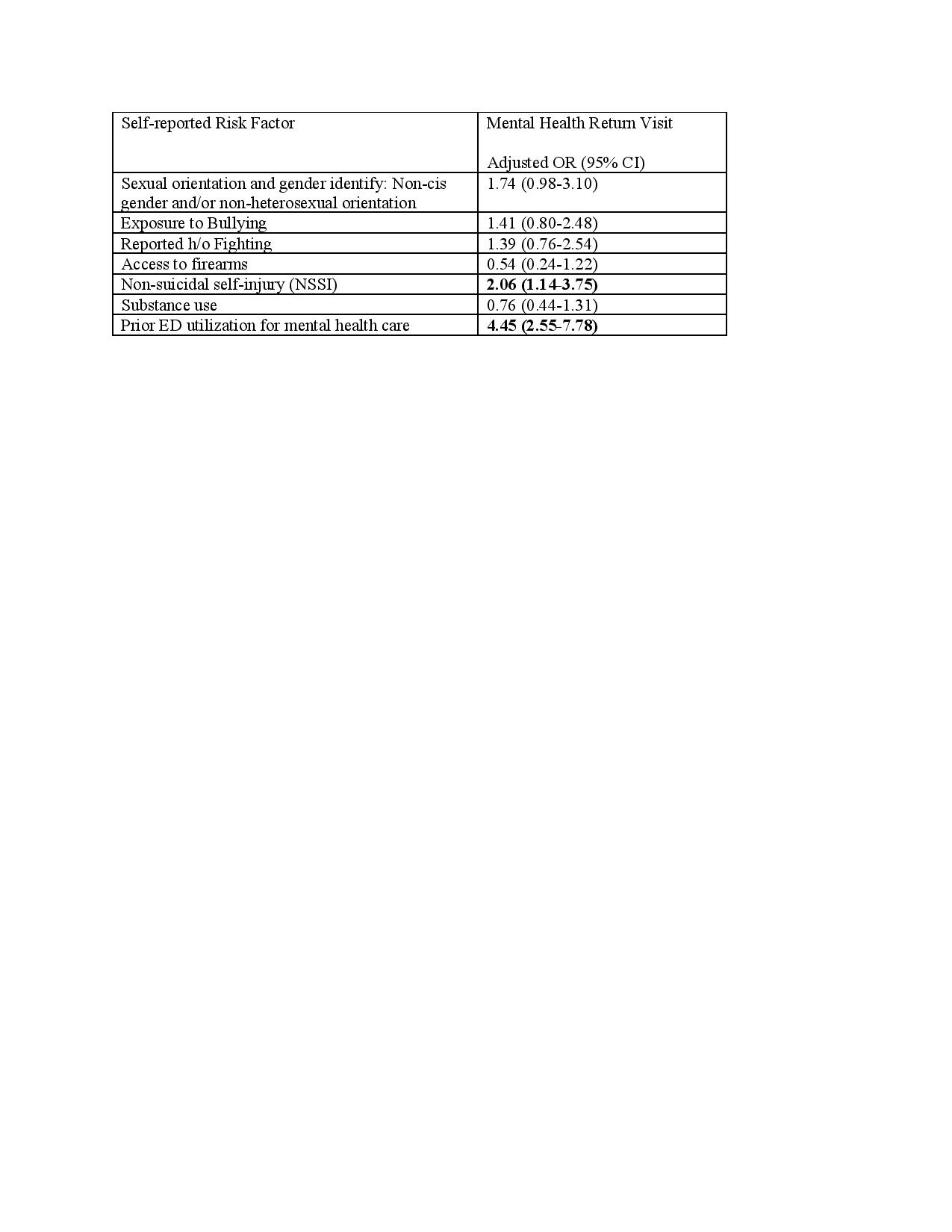
Results: ASQ suicide screening of 640 patients occurred, of whom 74 (11.6%) re-presented to the ED within 6 months for an acute mental health concern. The median time elapsed from ED discharge to mental health return was 42 days (IQR 26-100 days). Most (75.7%) return visits were for SI. A statistically higher proportion of youth re-presenting for ED mental health care were trans-male (6.8%) or gender non-conforming/gender non-binary (17.6%), gay or lesbian (12.2%), had experienced bullying (29.7% electronic, 33.8% in-person), or had a history of non-suicidal self-injury (NSSI) (Table 1). Adjusting for sexual orientation and gender identity, bullying, fighting, access to firearms, and substance use the odds of return were 2.06 times as likely (95% CI: 1.14, 3.75) among youth reporting prior NSSI and 4.45 times as likely (95% CI: 2.55, 7.78) among youth who had previously accessed the ED for mental health care (Table 2).
Conclusion(s): After adjusting for known risk factors for suicide, NSSI was the only self-reported risk factor associated with an increased odds of ED mental health return. Focused outpatient resources for youth with prior NSSI or previous ED utilization for SI may decrease return rates among youth screened at-risk for suicide.