Medical Education: Simulation & Technology
Medical Education 6: Simulation & Technology 1
536 - Single Center Experience with Implementing Cranial Point of Care Ultrasound as a Tool for Early Intracranial Hemorrhage Detection in Preterm Infants
Publication Number: 536.228

Sarah E. Kolnik, MB MBA (she/her/hers)
Assitant Professor of Pediatrics
University of Washington - Seattle Children's Hospital
Seattle, Washington, United States
Presenting Author(s)
Background: Point of care ultrasound (POCUS) is used as an extension of the physical exam that can improve a clinician’s diagnostic and even potentially prognostic abilities in real-time. Use of neonatal cranial POCUS to exploit these capabilities particularly for detection of intracranial hemorrhages (ICH) has not been standardized in US neonatal intensive care units.
Objective:
This study's aim was to track the quality of image acquisition by providers following early cranial POCUS training, and to assess if early cranial POCUS can assist with identifying ICH in at-risk preterm neonates.
Design/Methods: Observational single center cohort of infants born at ≤ 1250 g and/or ≤ 30 weeks’ gestation in at Level III NICU. Cranial POCUS was obtained by a trained practitioner (advanced practice practitioner, fellow, or attending) within the first 3 days after birth. Standard screening ultrasounds were done per unit protocol at 7-10 days after birth. Demographic and clinical data collection occurred retrospectively. Demographic variables of the included infants were portrayed with descriptive statistics using either median and interquartile range (IQR) or count and percentage. Metrics of image quality were assessed by a radiologist and ultrasound technician independently; ICH was diagnosed by a radiologist. A score of 1 (worst) to 5 (best) was assigned for depth, gain, and anatomy for each POCUS exam. Every 3-6 months quality metrics for each exam and tips for improvement were posted for review of participating providers. Analysis of trends in quality of POCUS images over time was done using a multinomial Cochran-Armitage test.
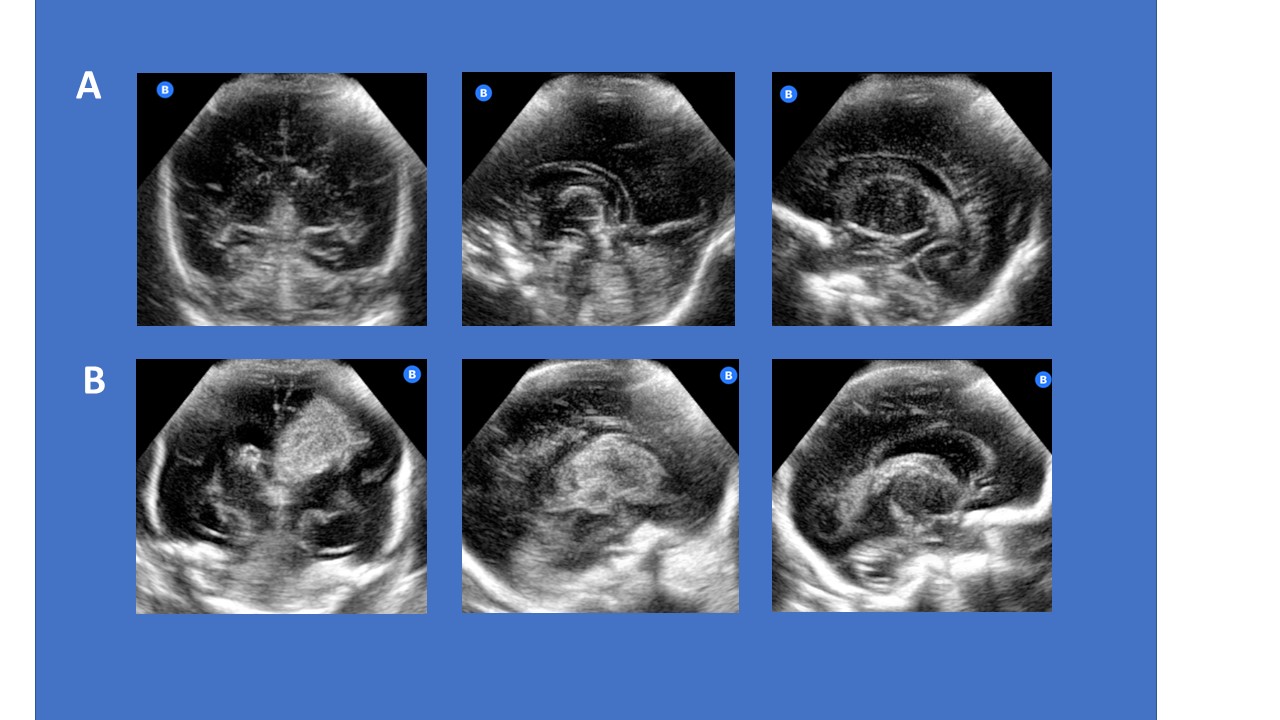
Results: 82 eligible infants were included in this analysis. Median age at POCUS exam was 14 hrs (IQR 7-22 hrs) and median age standard ultrasound was 7 days (IQR 5-10 days). Baseline characteristics of the study population are depicted in Table 1. Of the 82 infants, 9 had ICH detected by POCUS by 3 days after birth, of which 78% had detected ICH at 7-10 days after birth on routine ultrasound. Metrics of image quality depicted quarterly demonstrated an improvement in depth (p= 0.01), gain (p= 0.048), and quality of anatomy images captured (p < 0.001) over time (Figure 1). Although image quality varied, POCUS exams were able to capture whether ICH was present (Figure 2).
Conclusion(s): Cranial POCUS image acquisition improved significantly following care team training, providing clinicians the ability to diagnose ICH in a more expeditious manner. Future work temporally correlating ICH with clinical care provides a window of opportunity to devise better management and preventative measures.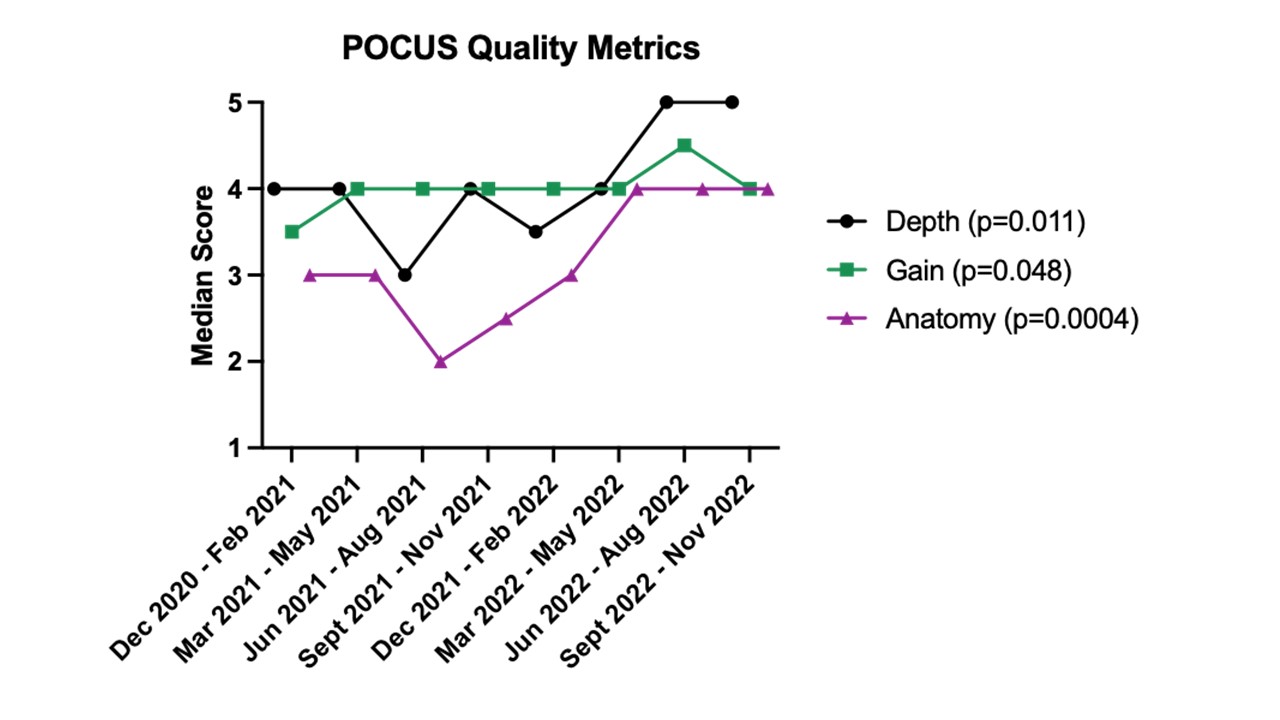
.jpg)
