Back
Background: Children with medical complexity (CMC) are a growing population who consume a disproportionate amount of inpatient and critical care resources. A substantial proportion of CMC have significant Neurologic Impairment (NI) resulting in disability. While it is known that patient disability can influence provider care practices, little is known about pediatric intensive care unit (PICU) clinicians’ views and experience caring for CMC with NI, including whether implicit biases affect the care of this population.
Objective: To explore and describe the experiences and beliefs of PICU providers caring for CMC, including how their experiences, beliefs, and biases may impact the medical care of CMC with NI as described by providers.
Design/Methods: We conducted a qualitative study of 20 PICU providers. Providers (12 attendings and 8 NPs) were recruited via purposive and snowball sampling from 7 PICUs across 6 states;10 participants were from the authors’ home institution and 10 from external PICUs. Semi-structured interviews were conducted over Zoom; recruitment continued until information power was achieved. Transcripts were coded using a constant comparative approach; relevant themes were analyzed using modified grounded theory.
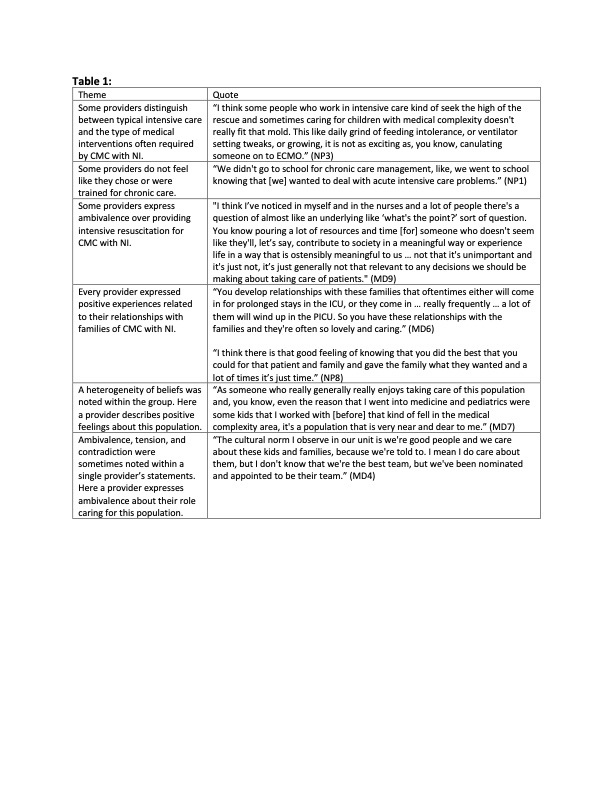
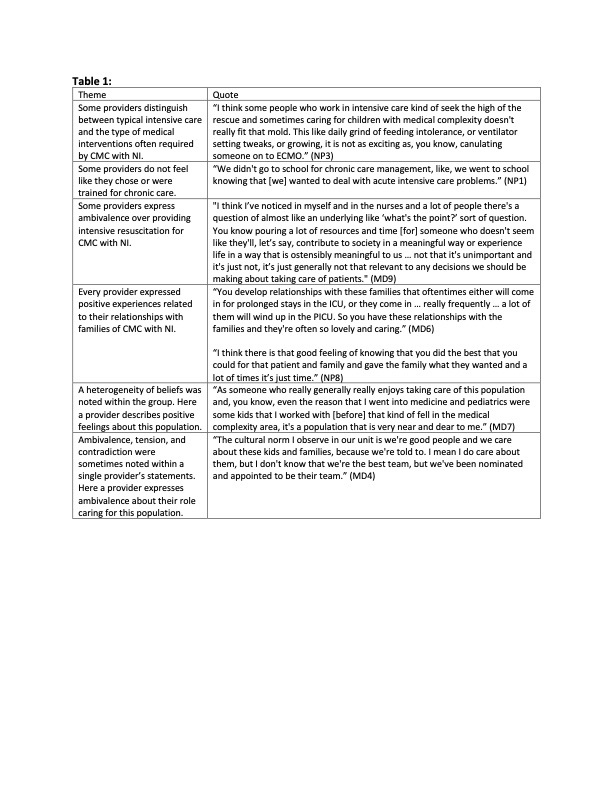
Results: We identified a strong theme of ambivalence about CMC with NI in many PICU providers’ perspectives (see Table 1). Treating chronic medical needs of CMC with NI in the PICU was described as not “true” critical care, and providers felt they did not choose, train for, or have resources to address chronic care issues like feeding intolerance or complex discharge planning. Some providers also expressed hesitancy about providing intensive resuscitation for severely neurologically impaired children. However, all providers expressed positive feelings and experiences in caring for the population related to connection with, service to, or empowerment of families. Overall, heterogeneity of attitudes (ranging from advocacy and compassion to moral distress and frustration) was noted among different providers, in the descriptions providers shared of their colleagues, and even within providers’ own statements.
Conclusion(s): Our study demonstrates PICU clinicians experience tension between their conception of their profession and caring for CMC with NI. We found that this population challenges the typical notion of what pediatric critical care represents, and that providers have a wide spectrum of emotions and beliefs about these patients. Understanding this relationship can provide insights for improved patient care and reduced provider burnout as the field adapts to this growing population.
Dr. Foster’s time, was supported by the National Heart, Lung, and Blood Institute (NHLBI) under 1K23HL149829-01A1 for research on care of children with medical complexity. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NHLBI or National Institutes of Health.
Critical Care
Critical Care 2
306 - “Nominated and Appointed” – PICU provider attitudes towards their care of medically complex, neurologically impaired children
Saturday, April 29, 2023
3:30 PM – 6:00 PM ET
Poster Number: 306
Publication Number: 306.205
Publication Number: 306.205
Elizabeth J.. Bleed, Ann & Robert H. Lurie Children's Hospital of Chicago, Chicago, IL, United States; Leonardo Barrera, Ann & Robert H. Lurie Children's Hospital of Chicago, Chicago, IL, United States; Mickayla Jones, Ann & Robert H. Lurie Children's Hospital of Chicago, Chicago, IL, United States; Seema K. Shah, Ann & Robert H. Lurie Children's Hospital of Chicago, Chicago, IL, United States; Megan Crowley-Matoka, Northwestern University, Chicago, IL, United States; Carolyn Foster, Northwestern University The Feinberg School of Medicine, Chicago, IL, United States

Elizabeth J. Bleed, MD, MA (she/her/hers)
Pediatric Critical Care Fellow
Ann & Robert H. Lurie Children's Hospital of Chicago
Chicago, Illinois, United States
Presenting Author(s)
Background: Children with medical complexity (CMC) are a growing population who consume a disproportionate amount of inpatient and critical care resources. A substantial proportion of CMC have significant Neurologic Impairment (NI) resulting in disability. While it is known that patient disability can influence provider care practices, little is known about pediatric intensive care unit (PICU) clinicians’ views and experience caring for CMC with NI, including whether implicit biases affect the care of this population.
Objective: To explore and describe the experiences and beliefs of PICU providers caring for CMC, including how their experiences, beliefs, and biases may impact the medical care of CMC with NI as described by providers.
Design/Methods: We conducted a qualitative study of 20 PICU providers. Providers (12 attendings and 8 NPs) were recruited via purposive and snowball sampling from 7 PICUs across 6 states;10 participants were from the authors’ home institution and 10 from external PICUs. Semi-structured interviews were conducted over Zoom; recruitment continued until information power was achieved. Transcripts were coded using a constant comparative approach; relevant themes were analyzed using modified grounded theory.
Results: We identified a strong theme of ambivalence about CMC with NI in many PICU providers’ perspectives (see Table 1). Treating chronic medical needs of CMC with NI in the PICU was described as not “true” critical care, and providers felt they did not choose, train for, or have resources to address chronic care issues like feeding intolerance or complex discharge planning. Some providers also expressed hesitancy about providing intensive resuscitation for severely neurologically impaired children. However, all providers expressed positive feelings and experiences in caring for the population related to connection with, service to, or empowerment of families. Overall, heterogeneity of attitudes (ranging from advocacy and compassion to moral distress and frustration) was noted among different providers, in the descriptions providers shared of their colleagues, and even within providers’ own statements.
Conclusion(s): Our study demonstrates PICU clinicians experience tension between their conception of their profession and caring for CMC with NI. We found that this population challenges the typical notion of what pediatric critical care represents, and that providers have a wide spectrum of emotions and beliefs about these patients. Understanding this relationship can provide insights for improved patient care and reduced provider burnout as the field adapts to this growing population.
Dr. Foster’s time, was supported by the National Heart, Lung, and Blood Institute (NHLBI) under 1K23HL149829-01A1 for research on care of children with medical complexity. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NHLBI or National Institutes of Health.