Emergency Medicine: All Areas
Emergency Medicine 3
48 - Outcomes of Clinical Event Debriefing Training for Pediatric Emergency Medicine Physicians
Publication Number: 48.112

Arianne Baker, MD (she/her/hers)
Fellow, Emergency Medicine
Boston Children's Hospital
Boston, Massachusetts, United States
Presenting Author(s)
Background:
Clinical event debriefing improves healthcare teams and patient outcomes but is infrequently done. Most pediatric emergency medicine (PEM) doctors are not trained to lead clinical debriefs. Online and in-person methods can train clinicians in debriefing skills.
Objective: To develop a debriefing curriculum comprised of a training module, simulation, and feedback, and evaluate the effect on performance, comfort, knowledge, and practice in clinical debriefs.
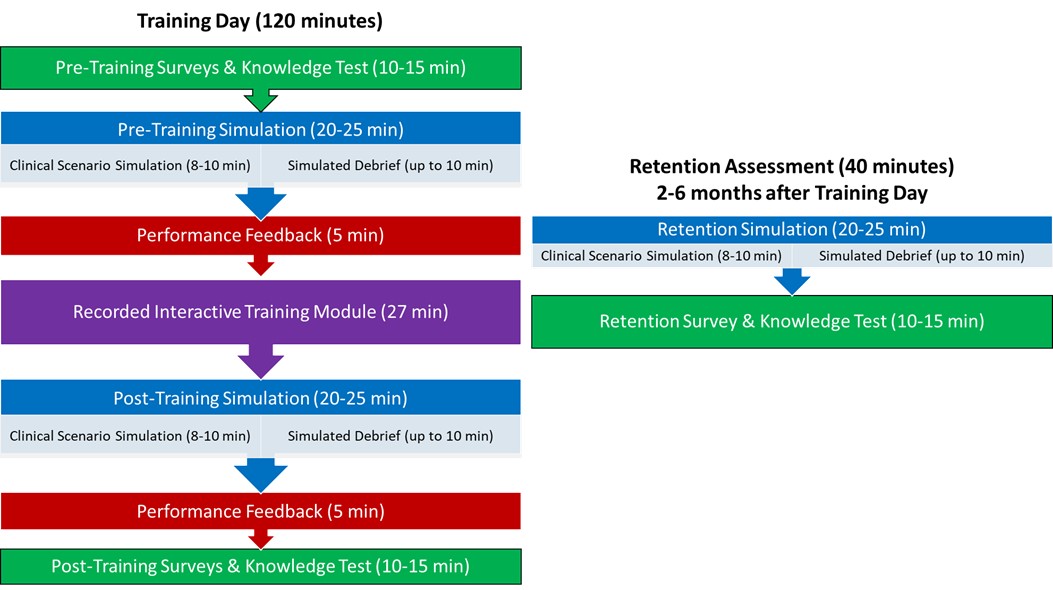
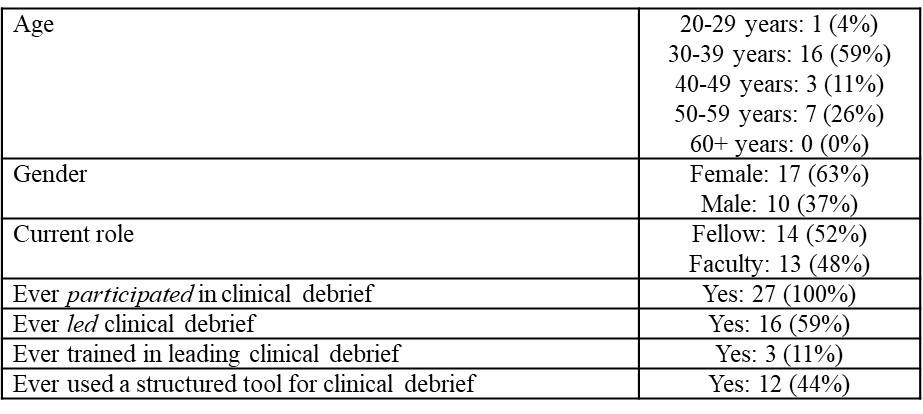
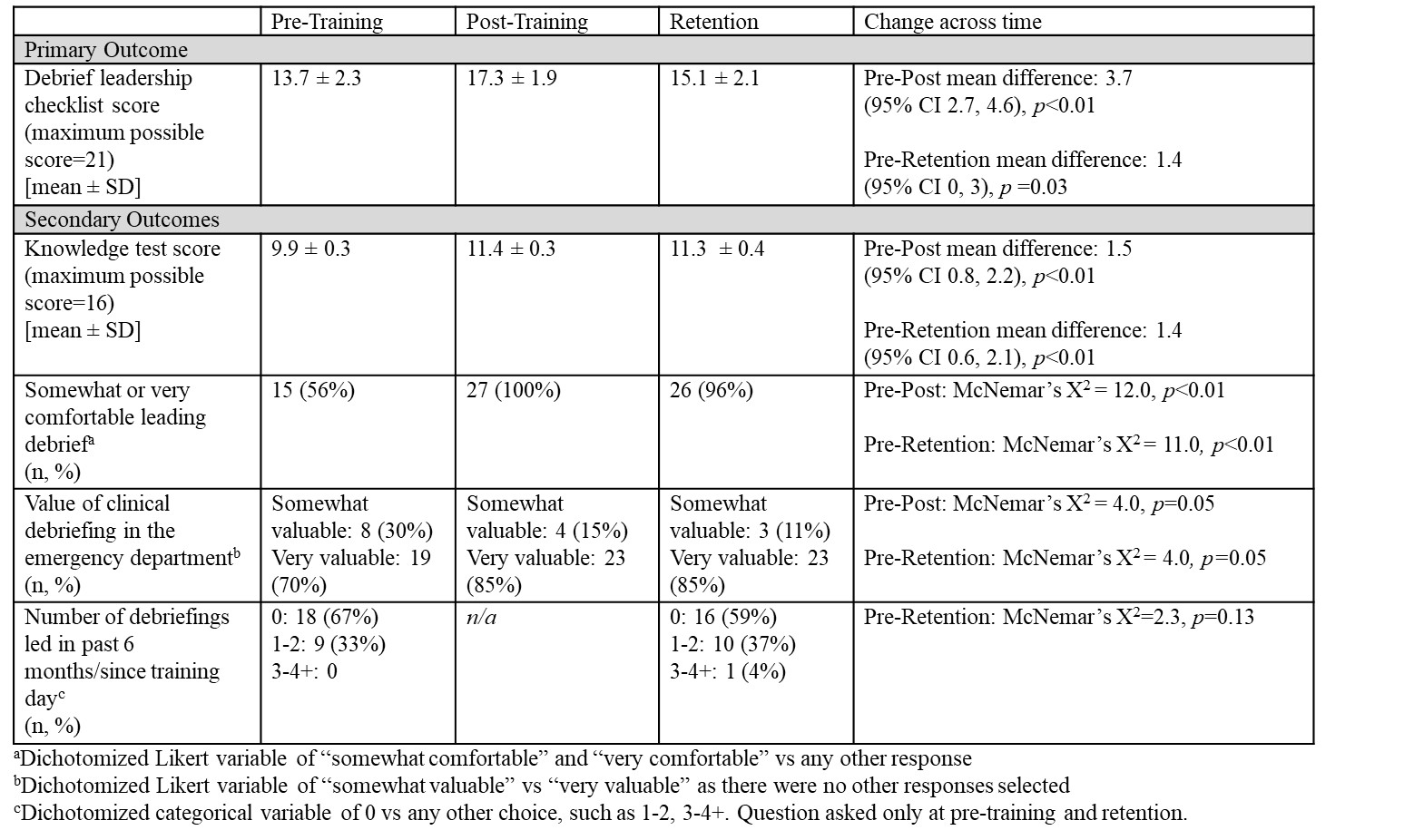
Design/Methods: This was a single-center prospective study of PEM fellows and faculty at a tertiary care pediatric hospital. The curriculum included simulation, feedback, and a training module (Fig. 1). Subjects completed one 2-hour session in which they led a standardized clinical simulation followed by a simulated clinical debrief (“pre-training”), received feedback, completed an interactive training module, then led another simulation and debrief with feedback (“post-training”). To assess retention over time, subjects completed a third simulation and debriefing 2-6 months after their training. At pre-training, post-training, and retention, subjects completed surveys measuring attitudes and experiences, a knowledge test, and a curriculum evaluation. A blinded, trained investigator watched video recordings of the debriefs and scored debrief leadership performance with a novel 21-item checklist. The primary outcome was debrief leadership performance using the checklist score. Secondary outcomes included comfort and knowledge regarding debriefs, curriculum evaluation, and changes in clinical practice. With 25 subjects, the power was 89% to find a 4-point change in performance. Paired t-tests were used for performance and knowledge scores and McNemar’s test for dichotomized Likert scale data.
Results: All subjects (n=27) completed the curriculum and retention assessment (Table 1). Debrief leadership performance, comfort leading debriefs, and debrief knowledge all significantly improved from pre- to post-training and improvements persisted through the retention assessment (Table 2). All participants found the simulations and feedback somewhat or very useful, and 96% found the training module somewhat or very useful. Most (67%) reported change in their practice leading clinical debriefs after training and all (100%) would recommend the training to other PEM physicians.
Conclusion(s): A hybrid clinical debriefing curriculum using simulation, feedback, and a training module led to sustained improvements in performance, knowledge, and comfort among PEM faculty and fellows. These results suggest that debrief training is feasible and useful for PEM physicians.