Medical Education: Simulation & Technology
Medical Education 6: Simulation & Technology 1
535 - Pilot RCT for repetitive simulation vs standard debrief on an interprofessional NICU team’s clinical performance when managing the acutely desaturated, intubated patient
Publication Number: 535.228

Tim Rogers, MD
Fellow
Nationwide Children's Hospital
Columbus, Ohio, United States
Presenting Author(s)
Background:
Neonates are prone to unplanned extubations (UEs), however, their recognition can be difficult. Navigating such situations is confusing as markers of intubation become unreliable and responding interprofessional (IP) teams share little combined training.
Nationwide Children’s Hospital has demonstrated high rates of UEs with exploratory simulations showing performance gaps in the management of acutely decompensating intubated patients. These included placing an over-reliance on CO2 detectors and poor communication among IP teams.
Simulation represents an ideal tool for further training in this area. It is less clear, however, which simulation strategies best promote acquisition and retention of knowledge and skills. Repetitive simulation (RS) is one such strategy in which events are followed by a targeted debrief with the opportunity to immediately repeat and improve upon mistakes. It has shown promise with pediatric residents but has unclear utility in inpatient IP team training.
Objective:
Assess feasibility of a simulation-based RCT using in-patient IP teams and compare the change in individual knowledge, technical skills and communication between repetitive practice simulation vs standard simulation on those team’s clinical performance when managing the acutely desaturated, intubated neonate.
Design/Methods:
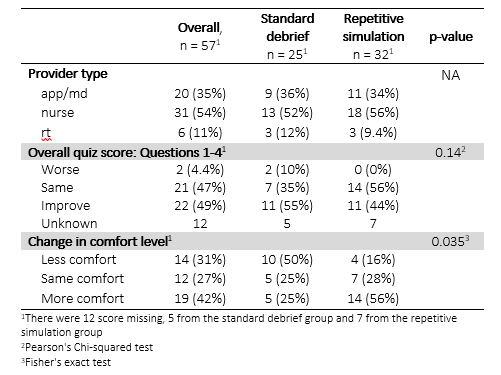
Inpatient IP teams participated in a simulated scenario of an intubated neonate experiencing an acute respiratory decompensation. Individuals were randomized to either standard debrief (STN) or a RS experience. Each team consisted of 2-3 participants (1 nurse practitioner or neonatal fellow, 1-2 neonatal nurses or 1 RT). All participants repeated the simulation 4-6 months later. Feasibility as well as individual knowledge, team technical skills and communication were assessed using a predefined scoring system (Table 1).
Results:
Overall, 57 providers comprising 20 teams participated in this pilot RCT. The study was feasible, with 47 providers comprising 19 teams returning for follow up. We did not see evidence of overall knowledge improvement, but did see evidence of increased comfort for the RS group (Table 2). Additionally, 100% of providers within the RS group felt such a format increased the educational value of the experience. Technical skills and communication are summarized in Figure 2.
Conclusion(s):
A simulation based RCT using in-patient IP teams managing an acutely desaturated, intubated neonate is feasible with the RS format possibly resulting in increased comfort of providers when compared to the STN format.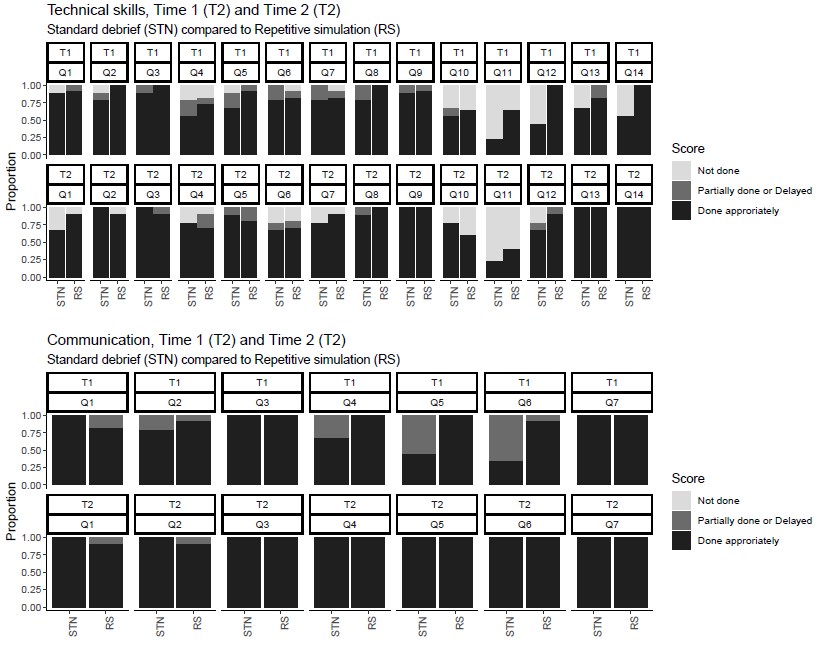
.png)