Medical Education: Simulation & Technology
Medical Education 6: Simulation & Technology 1
534 - Neonatal Multidisciplinary ECMO Simulation Program – Feasibility and Applicability
Publication Number: 534.228
- RJ
Romal K. Jassar, MBBS (she/her/hers)
Neonatologist
MassGeneral Hospital for Children
Boston, Massachusetts, United States
Presenting Author(s)
Background:
Neonatal ECMO has become a high acuity, low frequency event impacting provider experiences and patient outcomes. Mass General Hospital is a high volume ECMO center, but neonatal ECMO numbers fall under moderate volume. With decreasing incidence of ECMO use in non-cardiac critically ill neonates, we instituted a multidisciplinary in situ neonatal ECMO simulation program as an active learning tool.
Objective:
Multidisciplinary neonatal ECMO simulation is feasible and enhances provider experience with potential impact on patient care. We also aim to identify system issues during ECMO activation and initiation.
Design/Methods:
This is a survey based cross-sectional study design. High-fidelity simulation scenarios were conducted using a functional neonatal ECMO manikin with actual ECMO circuits, clinical space and multidisciplinary teams, standard EMR and utilization of standard checklists and processes for ECMO activation. Survey was designed for self-reporting of knowledge (learning), skills and attitudes (Likert scale 1-5 and open-ended questions): 1) learner reactions on simulation experience (Kirkpatrick level 1); 2) self-reflection of learning, clinical applicability, and impact on patient care (Kirkpatrick level 2). Data analysis conducted using descriptive statistics, ANOVA and word cloud for pattern recognition.
Results:
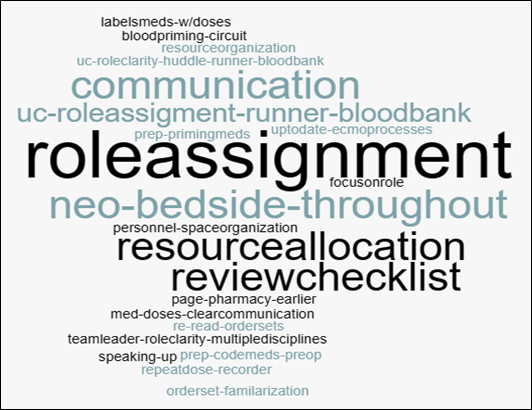
4 ECMO simulations were conducted from Oct 2020-2022. 43 learners completed the survey (40% RN, 28% MD/NP, 11% RT, 5% Pharmacist, 16% OR). 42% of learners had ≤10 years’ experience with NICU MD/NP (3 years) being least experienced vs pediatric surgeons (26 years). Figure 1 shows perception of: 1) learner reactions to simulation experience (quality, realism, debrief, clinical applicability); 2) self-report of learning, skills, and attitudes (impact on patient care, teamwork, skills, critical thinking, decision making). There was no statistical difference in above parameters based on years of experience (≤ 10 years vs > 10 years; all p values > 0.1). 74% of learners will modify practice and 7% reported no change in practice. Main system issues identified were delay in obtaining blood for circuit priming, medication labeling and checklist review. Figure 2 shows word cloud of learner identified practice modifications.
Conclusion(s):
High-fidelity neonatal ECMO simulation is feasible to conduct and improves learner experience and self-perception of knowledge and skills, with a positive attitude toward clinical applicability, practice modification which may potentially improve patient care and quality. ECMO simulation can identify system issues which may potentially impact patient care..png)