Neonatal Follow-up
NICU Follow Up and Neurodevelopment 5: Impact of Parents and Social Determinants of Health
165 - Neurodevelopmental outcome of very low birth weight infants in the Northern District in Israel
Publication Number: 165.363

Karen Lavie-Nevo, MD
NICU Director
Carmel medical center
Haifa, HaZafon, Israel
michal Molad, MD (she/her/hers)
Senior neonatologist
CARMEL MEDICAL CENTER
ATLIT, Hefa, Israel
Presenting Author(s)
Co-Author(s)
Background: Preterm infants are at high risk for short and long-term neurodevelopmental impairment in the neuro-motor, cognitive, language and behavioral domains. As rates of survival with and without morbidities vary significantly between countries, it is necessary to evaluate local rates of survival and neurodevelopmental outcomes to facilitate perinatal decision making and parental counseling, in cases of extreme preterm deliveries. However, no local study has been performed thus far in Israel
Objective:
In this retrospective study, we investigated the neurodevelopmental outcomes of very low birth weight (VLBW) preterm infants who were followed in one district of the largest health care organization in Israel.
Design/Methods:
The study population included all very low birth weight ( < 1500 g) preterm infants born between January 1st 2006 and December 31st 2016, who were followed in any of the 7 "Clalit" health service child development centers in Israel's Northern District; Haifa and Western Galilee counties. Data were retrospectively collected from the computerized medical record database.
Results:
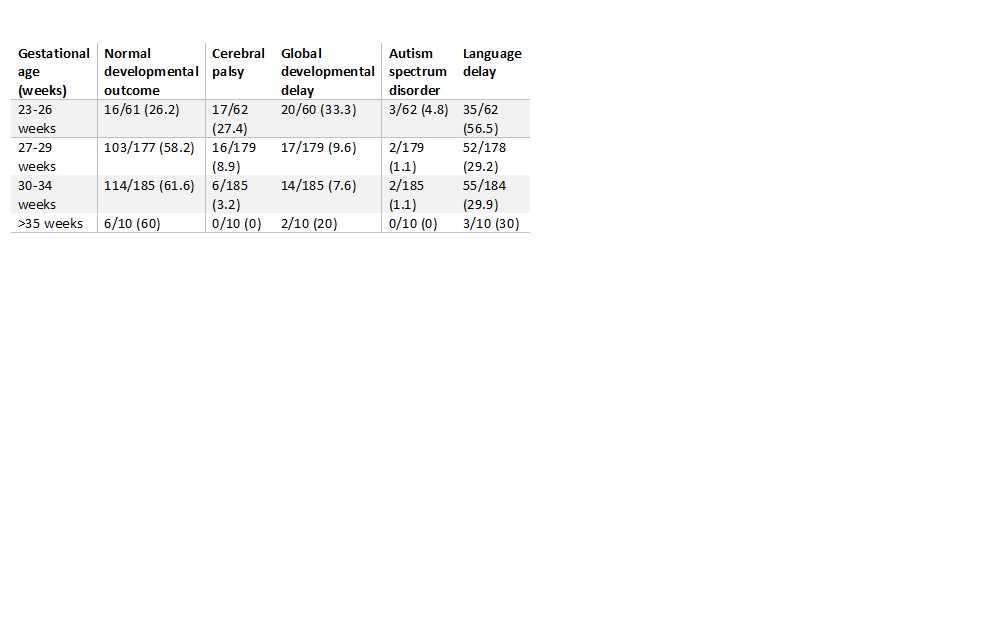
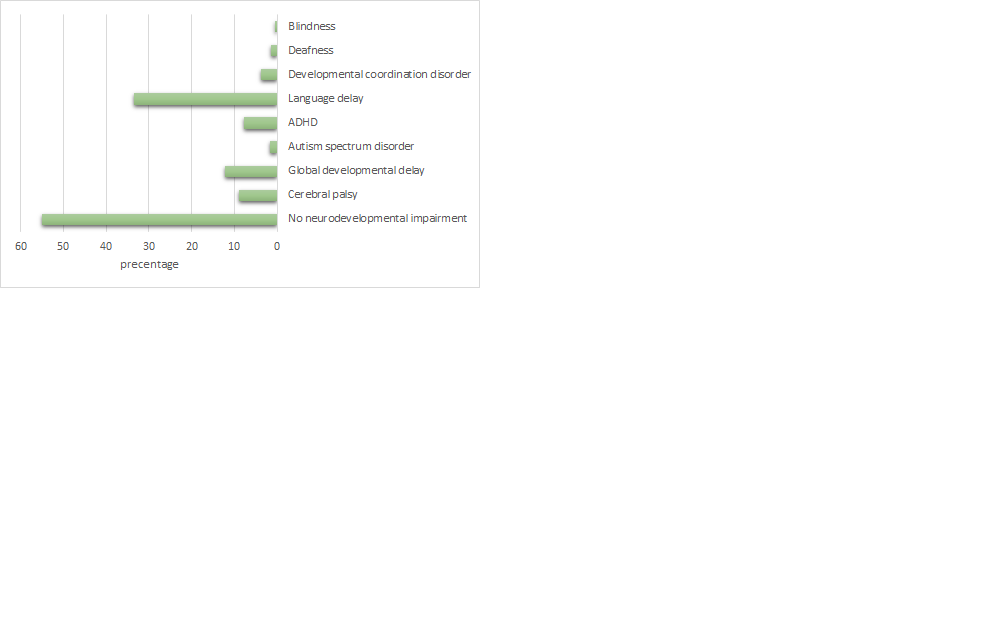
Out of 436 participants, 55.1% had normal developmental outcome. 8.9% were diagnosed with cerebral palsy (CP), 12.2% were diagnosed with global developmental delay (GDD), 33.4% had language delay, 1.6% were diagnosed with autism spectrum disorder and 7.8% had attention deficit and hyperactivity disorder (ADHD). Out of the extremely preterm infants born between 23-26 weeks of gestation (N=62), 27.4% had CP, 33.3% had GDD and 56.5% had language delay.
Only 26.2% of the preterm infants born between 23-26 weeks of gestation had normal development, compared to 58-61% of normal development in the other gestational age groups. .
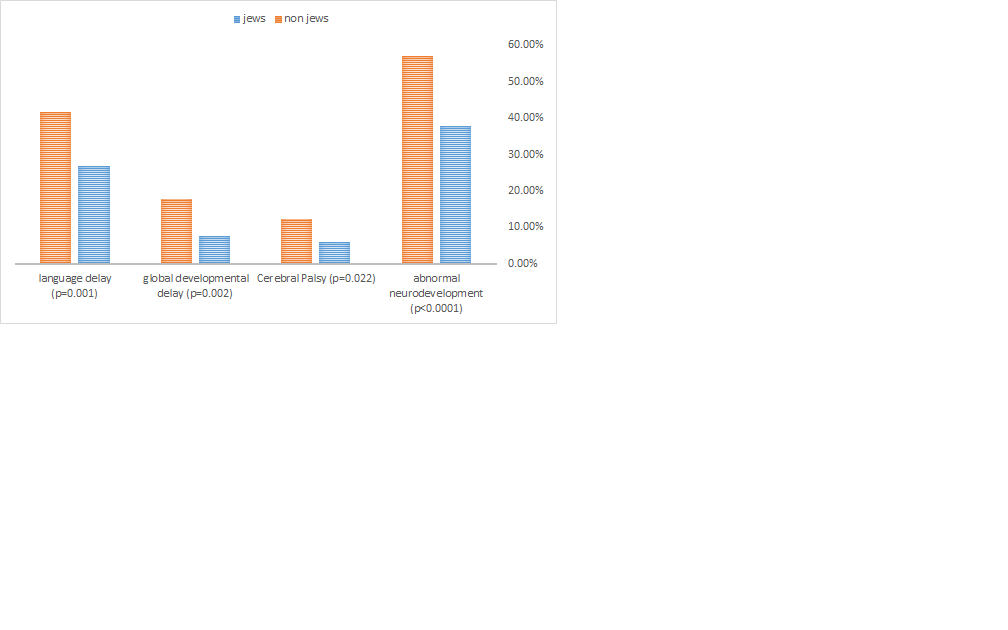
Comparing outcomes between Jews and non-Jews (mostly of Arab and Druze descent), we found a statistically significant difference in any abnormal neurodevelopment outcome, with a higher rate in non-Jews compared to Jews (57% vs. 37.8% respectively, p< 0.0001) which may be explained by differences in socioeconomic status, disparities in public health care and resources in distant rural areas, rate of consanguinity and compliance.
Conclusion(s):
We investigated local neurodevelopmental outcomes of VLBW preterm infants after 3 years of age and found a relatively high overall rate of CP, and a significant difference between Jews and non-Jews. This study emphasizes the need for an expanded and detailed local database of post-discharge outcomes, and for assessment of national health care resources and provision of care to preterm infants after discharge.