Neonatal Quality Improvement
Neonatal Quality Improvement 4
745 - Decreasing Antibiotic Exposure During Late Onset Sepsis Evaluations in a Level 4 NICU
Publication Number: 745.343
- KG
Kathleen Gibbs, MD (she/her/hers)
Neonatologist
Childrens Hospital of Philadelphia
Philadelphia, Pennsylvania, United States
Presenting Author(s)
Background:
Antibiotics are one of the most frequently used medications in the neonatal intensive care unit; we have 391 days of therapy per 1000 patient days/month. When prescribing antibiotics for suspected sepsis, we usually continue antibiotics until blood cultures are negative at 48 hours (h) of incubation. However, 90% of blood cultures are negative and most positive cultures result by 36h resulting in unnecessary antibiotic exposure. We have an existing and reliable huddle process at the time of sepsis evaluation which utilizes our clinical pathway for sepsis and documents clinical findings including initial steps in management.
Objective:
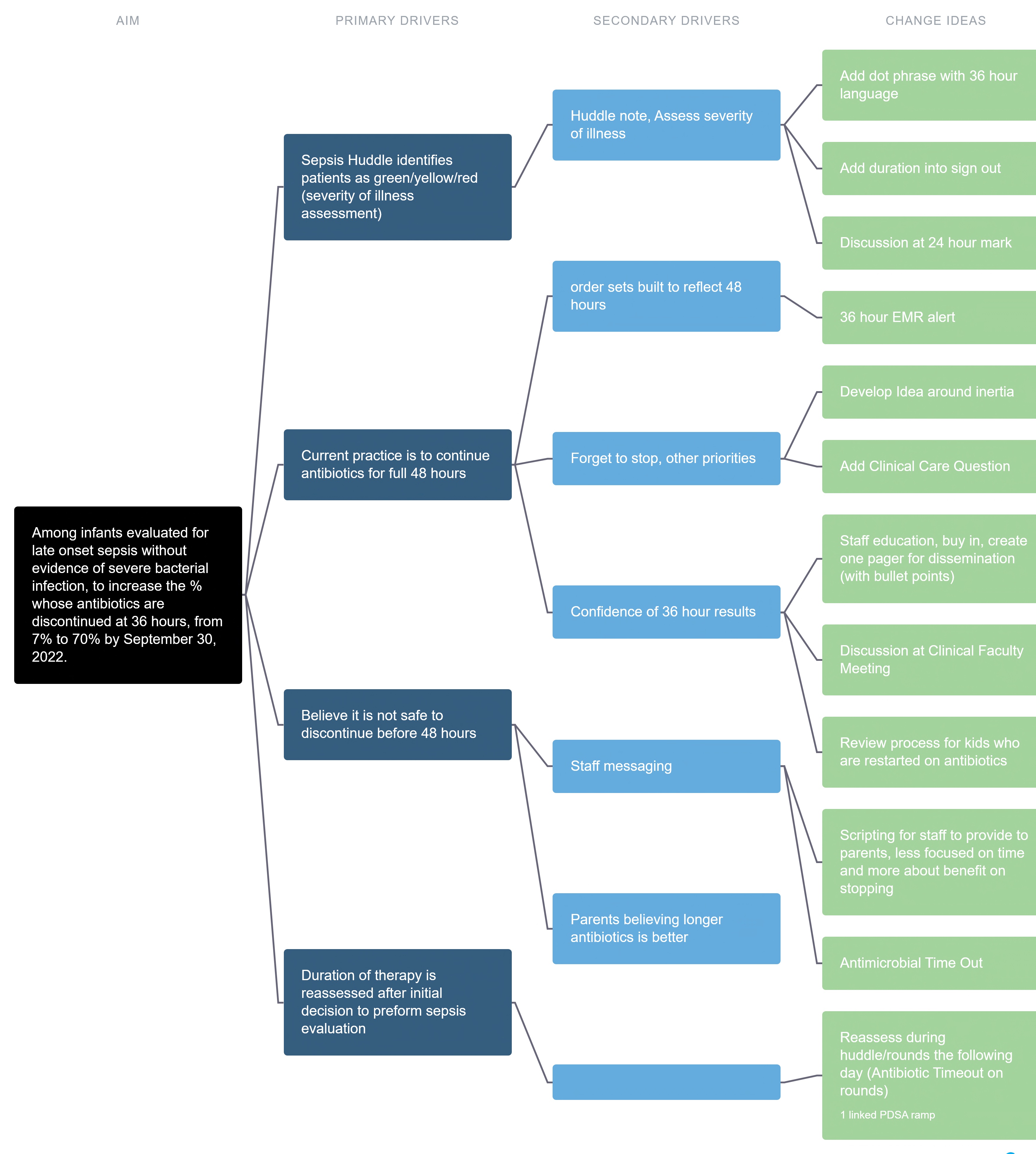
Among infants evaluated for late onset sepsis without clinical evidence of severe bacterial infection, we aimed to increase discontinuation of antibiotics within 36h, from 7% to 70% by September 30, 2022.
We hypothesize this will safely decrease antibiotic utilization and healthcare waste.
Design/Methods: Our driver diagram is in Figure 1. The outcome measure is the % of antibiotics stopped at 36h among patients who had a late onset sepsis evaluation. This measure was stratified by race/ethnicity. The outcome measure annotated with PDSA cycles is depicted in a statistical process control p chart (Figure 2). Documentation of 36h intended duration served as a process measure with a median of 40%. A PDSA cycle that revised a dot phrase to include intended duration of antibiotics (related to the process measure) is shown in Figure 3.
The % of cultures yielding a positive result after 36h antibiotic discontinuation served as a balancing measure. Additional outcome measures include nursing and pharmacy time for doses neither prepared nor administered.
Results:
Antibiotic discontinuation at 36h increased from 7% to 50% (Figure 2). Stratification by race/ethnicity identified all groups had centerline increases in discontinuation rates. No positive cultures resulted after stopping antibiotics. Nursing hours per month spent administering antibiotics were 3.5 hours fewer if discontinued at 48 vs 36 h (8.5 vs 5h). Later PDSA cycles utilized the electronic medical record to improve reliability of process measures.
Conclusion(s):
Among critically ill infants evaluated for late onset sepsis in our level 4 NICU, antibiotics were commonly discontinued at 36h of negative results without evident harm. Our efforts decreased time spent by both nursing and pharmacy colleagues preparing and administering antibiotics and exposed infants to fewer antibiotic doses. Stratifying measures by race/ethnicity is a method to assess for the introduction of inequity during improvement work. 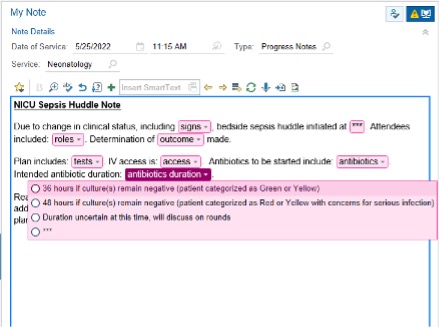
.jpg)
