Neonatal Pulmonology
Neonatal Pulmonology 2: BPD Clinical
263 - Non-Modifiable and Modifiable Risk Factors for Tracheostomy in Preterm Infants
Sunday, April 30, 2023
3:30 PM - 6:00 PM ET
Poster Number: 263
Publication Number: 263.34
Publication Number: 263.34
Brandon S. Dudeck, University of Maryland Children's Hospital, Hazle Township, PA, United States; Wendy Sun, University of Maryland School of Medicine, Rockville, MD, United States; Eunsung Cho, University of Maryland School of Medicine, Baltimore, MD, United States; Rose M. Viscardi, University of Maryland School of Medicine, Timonium, MD, United States

Brandon S. Dudeck, MD
Neonatology Fellow
University of Maryland Children's Hospital
Hazle Township, Pennsylvania, United States
Presenting Author(s)
Background: CLD, GA< 30 wk, ELBW (< 1000 g) and prolonged IMV are risk factors for tracheostomy in preterm infants. Determining additional risk factors may identify infants at high risk for tracheostomy and lead to development of possible risk mitigation strategies.
Objective: To identify modifiable and non-modifiable risk factors for tracheostomy among infants born ≤32 wk GA.
Design/Methods: We conducted a retrospective matched case-control study of preterm infants ≤32 wk GA admitted to single level IV NICU between 2000-2018. Two controls per tracheostomy case were identified and matched for GA ±1 week, BW±100g and NICU admission within the same year. Exclusion criteria included congenital airway anomalies and neurologic etiology of ventilator-dependence. Demographics, perinatal factors, NICU comorbidities, LOS, and numbers of intubations, extubations, and unplanned extubations were recorded. Statistical analysis included Student t test and Mann-Whitney test for normally and non-normally distributed continuous variables, respectively, and Fisher’s exact test for categorical variables. Odds ratios and 95% CI were calculated by a conditional (fixed-effects) logistic regression.
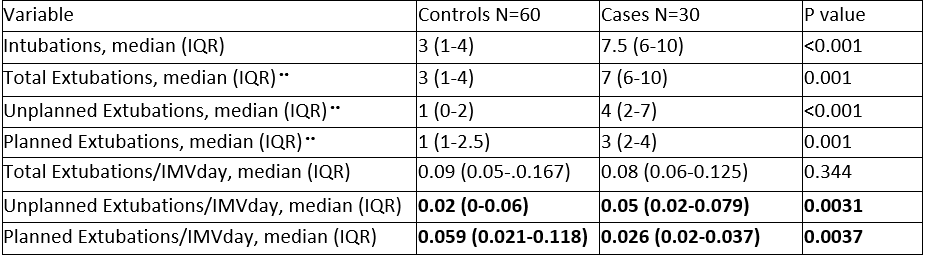
Results: 30 tracheostomy cases and 60 matched controls were included. Cases were GA 26.1±2.1 wks and BW 773±217g (mean±SD). Matched controls were GA 26.3±2.4 wks and BW 773±217g. Cases were 158d (127-183) of age and 48 wk (44.6-55) post-menstrual age (PMA) at time of tracheostomy following 92d (64-134) IMV; median (IQR). Risk factors significantly associated with tracheostomy included male sex, outborn birth, SGA, pulmonary hypertension, and culture-confirmed sepsis (Table 1). Duration of ventilation, LOS, and PMA at discharge were longer for tracheostomy cases compared to matched controls. The number of intubations, extubations (planned and unplanned) as well as planned and unplanned extubations adjusted for duration IMV were significantly higher in cases than controls (Table 2).
Conclusion(s): Non-modifiable risk factors for tracheostomy in preterm infants ≤32 wk include male sex, SGA, and pulmonary hypertension. Potential modifiable risk factors include sepsis, prolonged invasive ventilation, and unplanned extubations. Providers should consider these risk factors when counseling parents. Strategies to minimize tracheostomy risk should target high-risk infants.
.png)