Neonatal Neurology: Clinical Research
Neonatal Neurology 6: Clinical 6
121 - Duration of Hypotension and Risk of Severe Intraventricular Hemorrhage in Periviable Infants
Sunday, April 30, 2023
3:30 PM - 6:00 PM ET
Poster Number: 121
Publication Number: 121.338
Publication Number: 121.338
Leah B. Staines, University of South Florida, Wesley Chapel, FL, United States; Kaitlyn Steward, University of South Florida, St. Petersburg, FL, United States; J. Blaine John, Pediatrix Cardiology Associates, St. Joseph's Children's Hospital, University of South Florida, Tampa, FL, United States; Jaime Flores-Torres, University of South Florida, Tampa, FL, United States; Karen M. Wickline, University of South Florida, Tampa, FL, United States

Leah B. Staines, MD (she/her/hers)
Fellow
University of South Florida
Wesley Chapel, Florida, United States
Presenting Author(s)
Background: Intraventricular hemorrhage (IVH) is a major neonatal complication of infants born before 26 weeks gestation. Factors that cause fluctuation in cerebral blood flow including hypotension, especially during the first week of life, are risks for IVH.
Objective: Understanding the relationship between hypotension duration and risk of severe IVH could help guide our management of a hypotensive premature infant, especially when considering timing of intervention.
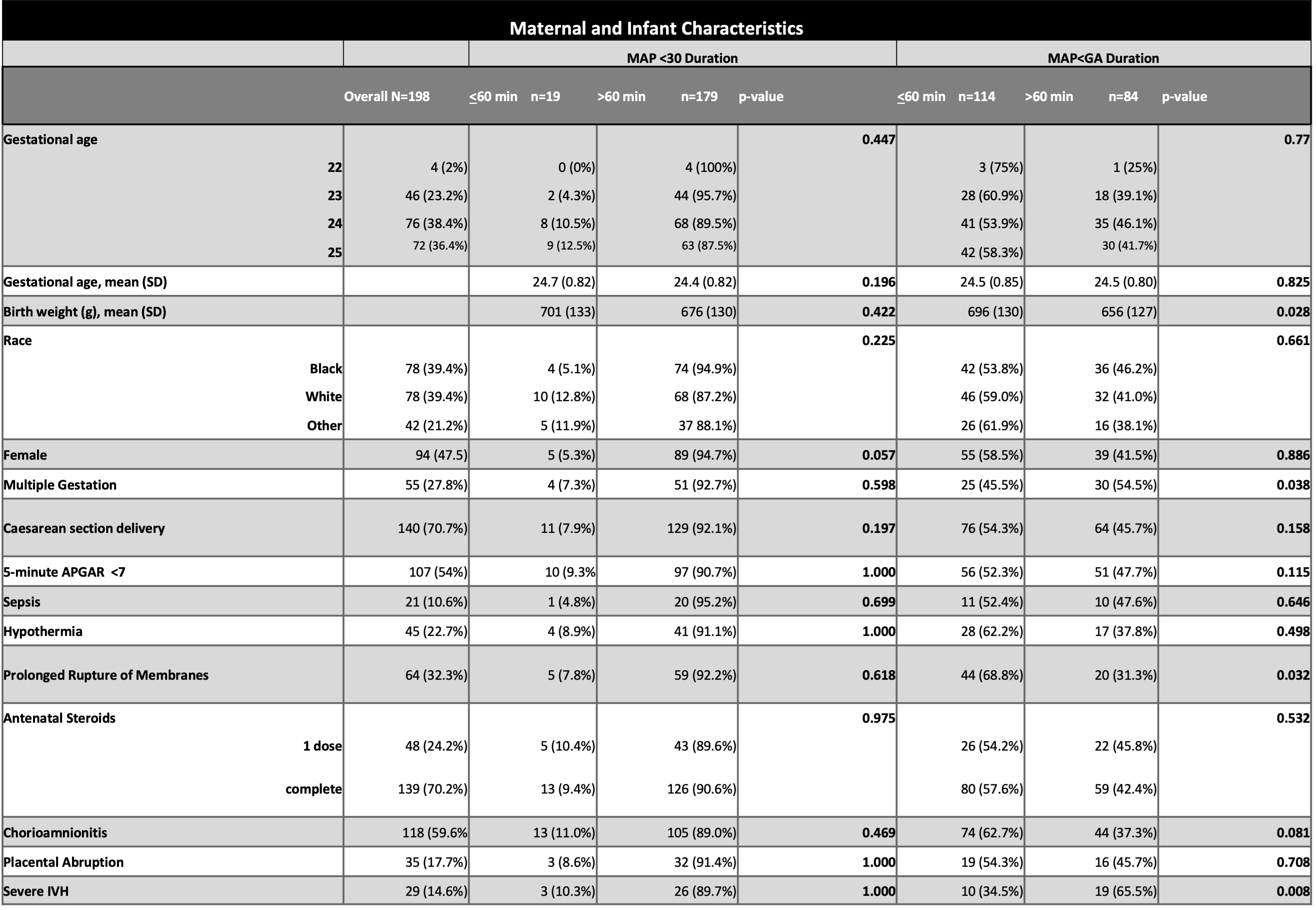
Design/Methods: We performed a single-center retrospective cohort study. All liveborn infants with < 26 weeks completed gestation between the years 2013 and 2020 were eligible for inclusion. Infants with multiple severe congenital anomalies, brain anomalies, severe congenital heart disease, death before head ultrasound, and outborn infants were excluded. Hourly mean arterial pressures (MAP) for the first 72 hours of life were extracted for each infant. Data for duration of hypotension was collected based on two commonly accepted definitions of hypotension: MAP below gestational age (MAP< GA) and MAP below 30 (MAP< 30). The diagnosis and severity of IVH was assessed using head ultrasound at 7 days of life. Chi-squared test or Fisher’s exact test was used to analyze categorical variables and independent sample T-test for continuous variables. We performed a multivariable logistic regression analysis to assess crude and adjusted associations between outcomes and predictive factors.
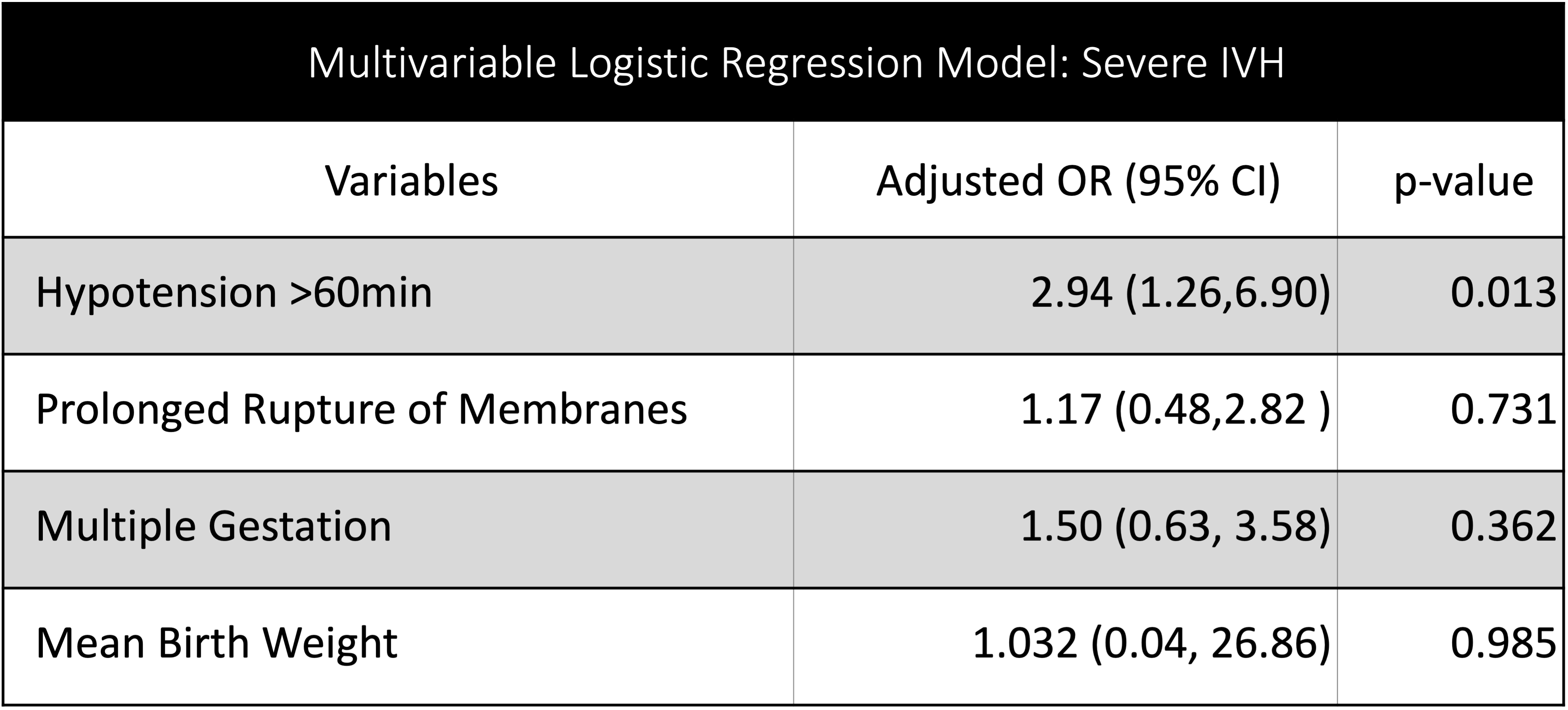
Results: 198 infants met criteria for inclusion. Infants that were hypotensive for longer than 60 consecutive minutes had higher severity of IVH (p=0.008) when using a MAP< GA as the definition of hypotension. In our univariate analysis, mean birth weight, multiple gestation, and prolonged rupture of membranes were significantly associated with longer duration of hypotension (MAP< GA for longer than 60 minutes). There were no significant findings when using the MAP< 30 definition. A multivariable logistic model revealed hypotension duration longer than 60 minutes to be independently predictive of IVH severity.
Conclusion(s): Hypotension (MAP< GA) for longer than 60 consecutive minutes is associated with higher severity of IVH in periviable infants.
.png)