Medical Education: Medical Student
Medical Education 12: Student 2
565 - Impact of Medical Improvisation Training on Medical Students’ Experience with Communication on Clinical Rotations
Publication Number: 565.326
- SK
Stephanie K. Kukora, MD (she/her/hers)
Assistant Professor, Neonatology and Bioethics
Children's Mercy Hospital
Kansas City, Missouri, United States
Presenting Author(s)
Background:
Effectively preparing students to communicate with patients, families, and teams is a challenge in medical education. Although techniques from Medical Improvisation (MI) have been proposed to teach communication skills in this context, limited evidence exists regarding how MI training impacts real-life interactions.
Objective:
To provide an MI-based educational training in the pre-clinical year and gather medical students’ reflections following one year of clinical rotations.
Design/Methods:
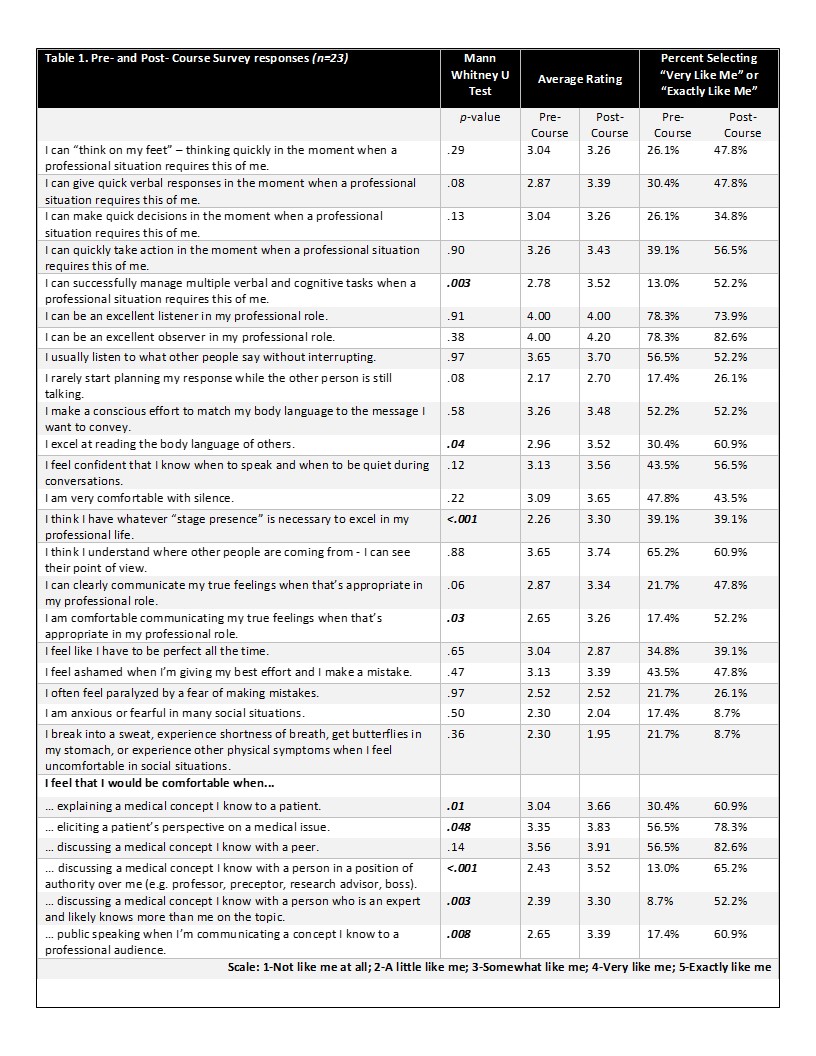
We recruited medical student volunteers to participate in an established curriculum (Watson, 2011), lasting 2 hours per week for 5 weeks, prior to beginning clinical rotations. Participants completed evaluations before and after the course, which included structured and open-ended questions about their experience and self-perceived impact. We conducted semi-structured interviews one year later after students completed core clinical rotations and performed thematic analysis on transcripts.
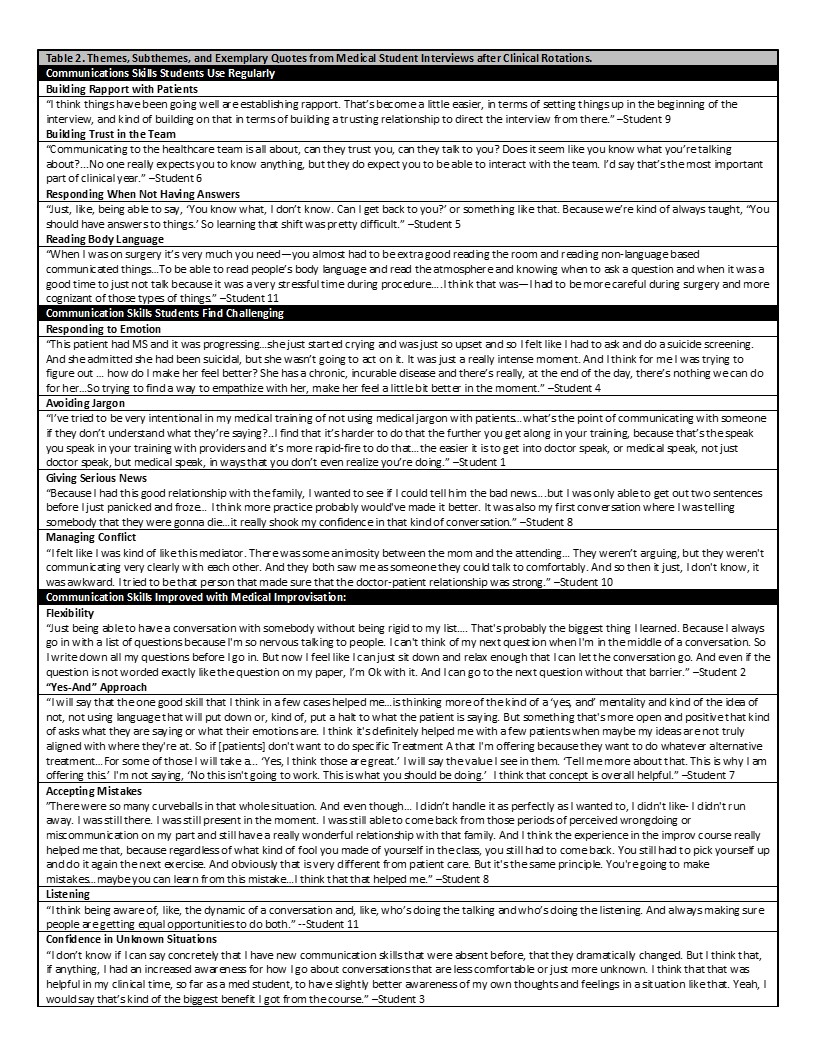
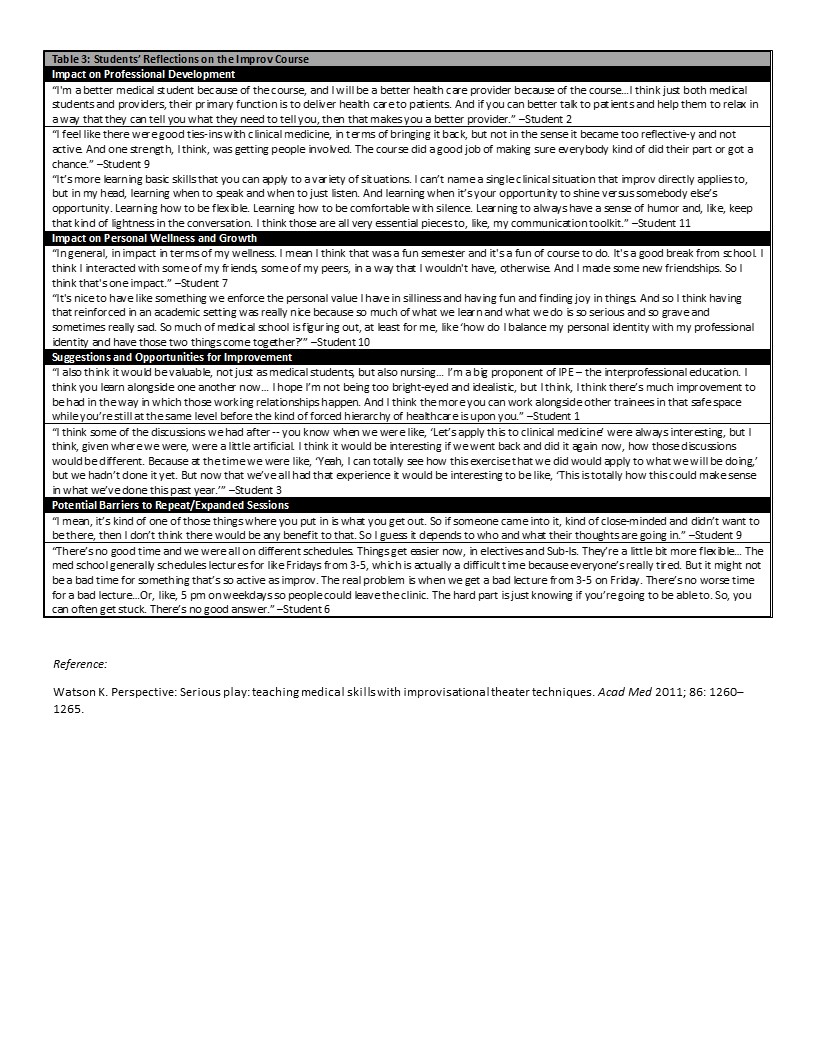
Results: 23 of 24 recruited students completed the course and surveys. Pre/post-course comparison survey data (Table 1) show significant improvements in reported comfort with different communication situations. 35% of students ranked the course as “above average” and 65% ranked it as “excellent.” 11 students (48%) participated in follow-up interviews. All interviewees reported enjoying the course and would recommend it. Major themes included: “regularly used communication skills” (subthemes: building rapport with patients, building trust with the team, responding when not having answers, and reading body language); “challenging communication skills” (sub-themes: responding to emotions, avoiding jargon, giving serious news, and managing conflict); and “skills improved by MI” (subthemes: flexibility, “Yes-and” approach, accepting mistakes, listening, and confidence in unknown situations). Quotes are reported in Table 2. Few students recalled specific exercises, but many felt MI was helpful to their professional development and gave them “tools” for challenging conversations in real-life practice. They also reported benefits in personal growth/wellness and building friendships. Students suggested repeating MI sessions after clinical rotations and MI for interprofessional collaboration but noted attitude of participants and time constraints as barriers. Quotes are listed in Table 3.
Conclusion(s): MI shows promise as an enjoyable and effective communication skills training approach for medical students.