Medical Education: Simulation & Technology
Medical Education 9: Simulation & Technology 2
531 - Using Virtual Reality Simulations to Support Motivational Interviewing Skills Among Medical Students Entering Pediatrics Residency
Publication Number: 531.327

Daniel G. Young, MD (he/him/his)
Pediatric Hospitalist Fellow
Washington University in St. Louis School of Medicine
Saint Louis, Missouri, United States- TA
Presenting Author(s)
Co-Author(s)
Background: The COVID-19 pandemic required educators to provide meaningful clinical experiences to distanced learners. Motivational interviewing (MI), a collaborative communication style to strengthen one’s commitment to change, is an essential skill for physicians. Virtual patient simulations, delivered via video teleconferencing, are an alternative to traditional standardized patients and have been used to train pediatric residents in communication skills. However, little is known about the use of virtual patients to train medical students in communication skills, specifically MI.
Objective:
1) To assess the impact of a virtual patient communication curriculum, delivered via video teleconferencing, on MI skill confidence for fourth-year medical students entering pediatrics. 2) To evaluate the acceptability and feasibility of our curriculum delivered via video teleconferencing to outside medical schools.
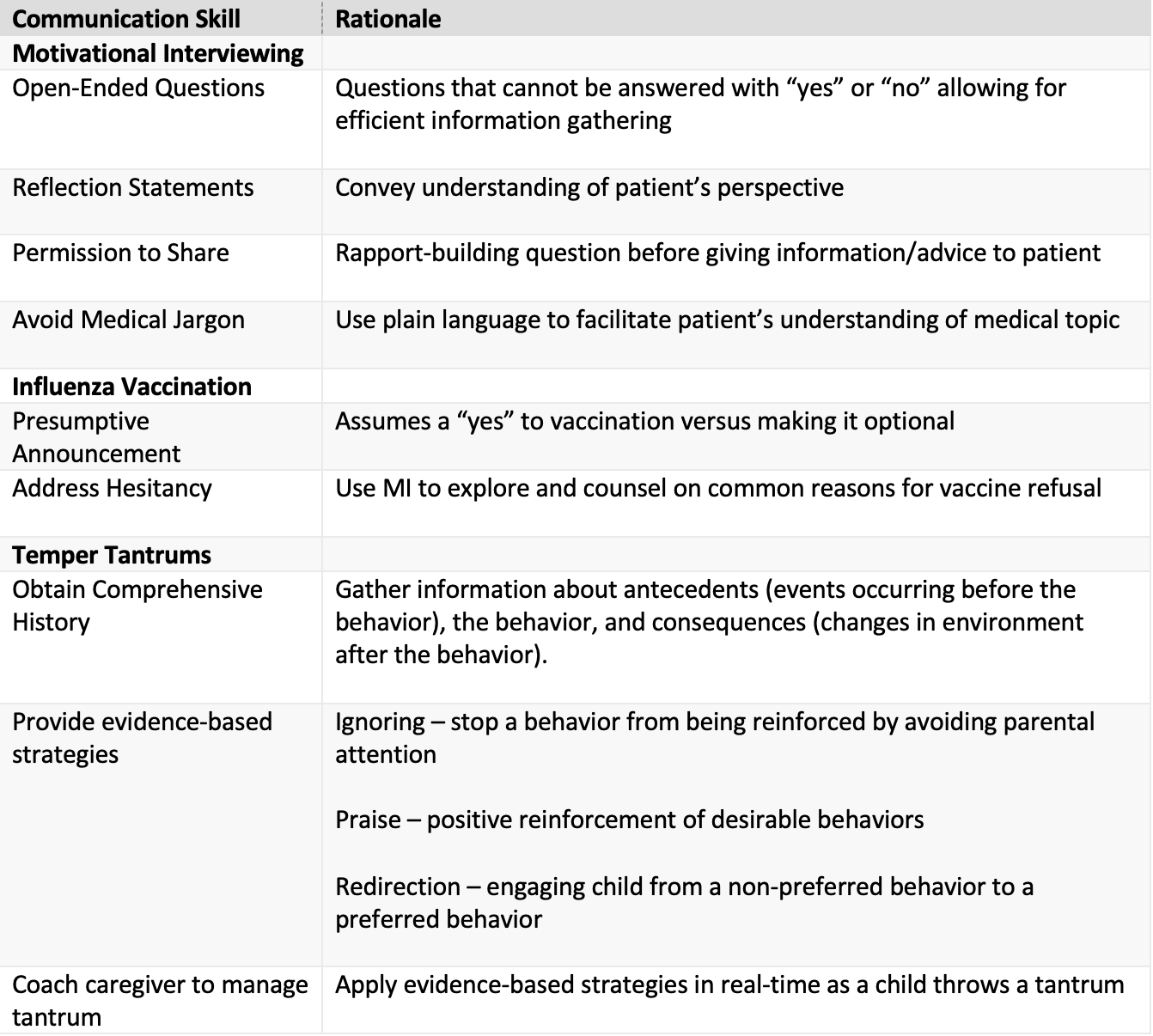
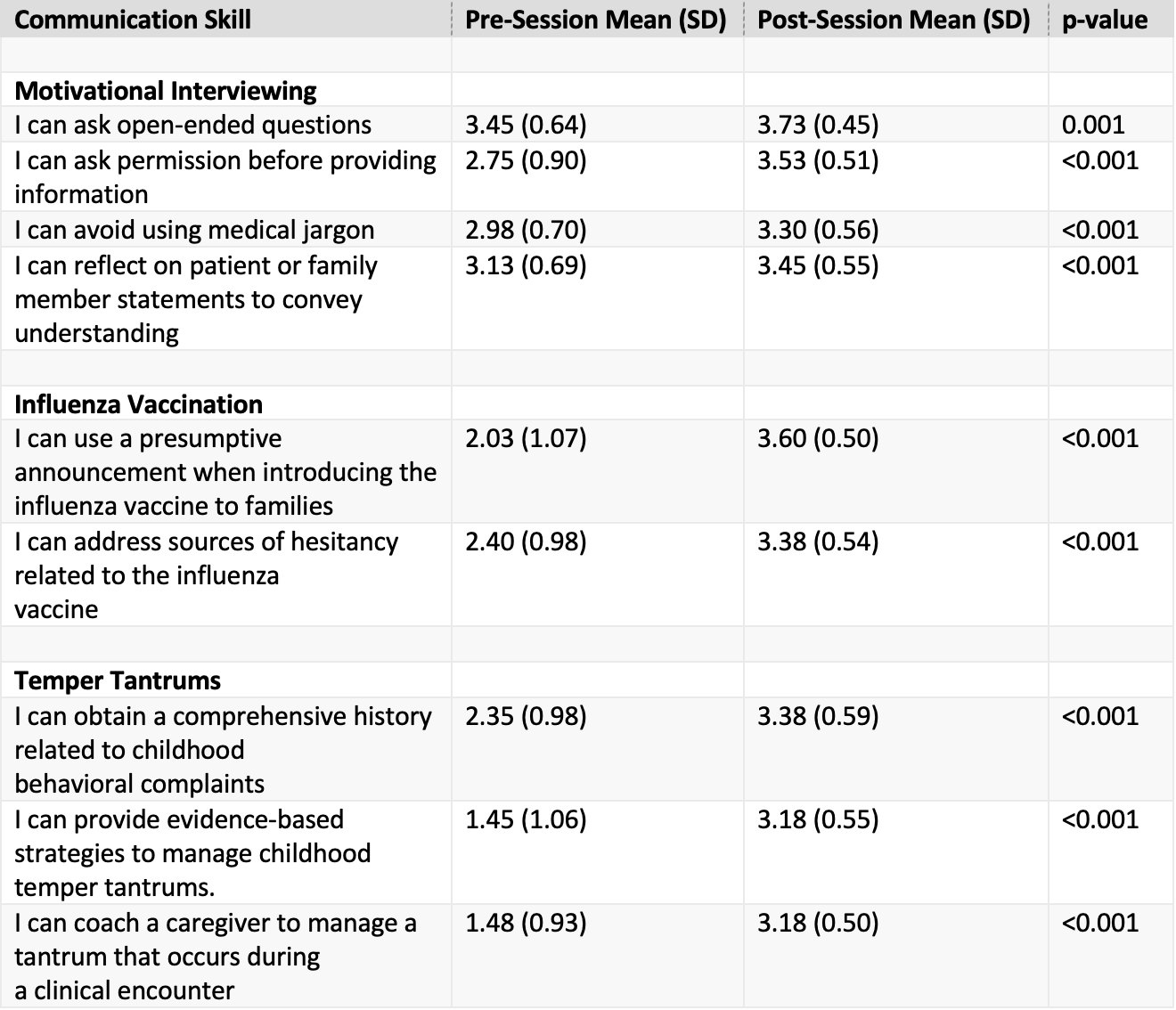
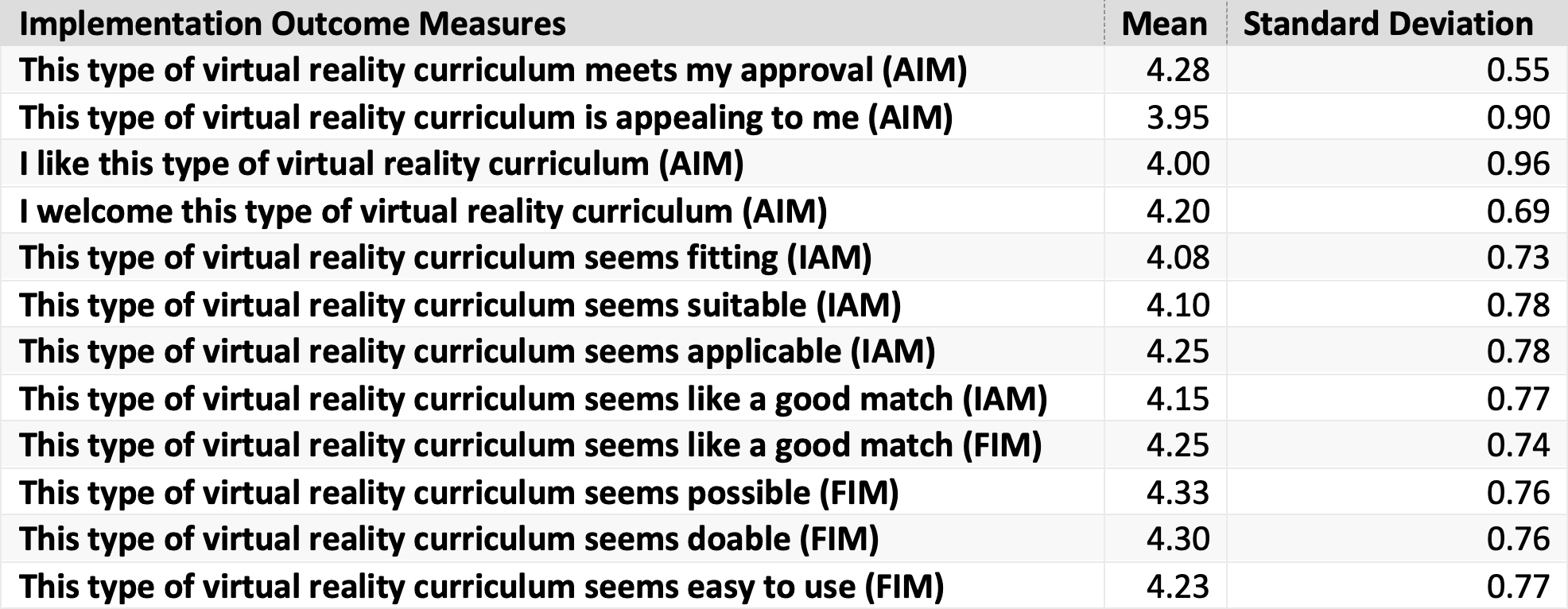
Design/Methods: Participants included fourth-year medical students enrolled in a pediatric intern-readiness “bootcamp” curricula at four United States medical schools in Spring 2022. The virtual reality (VR) curriculum was a two-hour mixed didactic/virtual simulation experience with real time feedback focused on practicing MI competencies in the context of two common and challenging topics for early trainees: addressing influenza vaccine hesitancy and behavioral health counseling. These topics were identified through feedback from residents and program directors. A retrospective pre/post Likert scale survey measured learners’ confidence related to curricular communication skills (0=not at all confident, 4=very confident) (Table 1). Paired t-tests compared changes in confidence ratings. Descriptive statistics assessed acceptability and feasibility of the curriculum (1=completely disagree, 5=completely agree).
Results:
Forty of 53 students (75%) completed the survey. Most students identified as a woman (65%) and white (75%). There was a statistically significant increase in students’ self-reported confidence in MI skills, including using reflection statements, asking permission before sharing information, and avoiding medical jargon (all p< 0.001) (Table 2). Students agreed that the curriculum was highly feasible, acceptable, and appropriate (Table 3).
Conclusion(s): VR patient simulations via video teleconferencing may provide a feasible distanced platform for teaching MI skills to medical students. Next steps include evaluating higher-level learner outcomes, such as behavior change during patient encounters, and training more VR facilitators to increase reach of the curriculum.