Neonatal Infectious Diseases/Immunology
Neonatal Infectious Diseases/Immunology 4
419 - Evolving Trends and Geographic Differences in Neonatal Infections: A 10-year Retrospective Cohort Study of North American Level IV Neonatal Intensive Care Units
Publication Number: 419.335
.jpg)
Yo Nishihara, MBBS (he/him/his)
Neonatal Fellow
University of Colorado School of Medicine
Aurora, Colorado, United States
Presenting Author(s)
Background:
Intrapartum antibiotic use has reduced early onset Group B Streptococcus (GBS) infections across neonatal intensive care units (NICUs). However, there is concern for a paradigm shift in the emergence of non-GBS pathogens. Additionally, variability in antimicrobial prescribing practices across NICUs nationally may give rise to regional differences in identified pathogens. Level IV NICUs have a diverse population of infants, including those with multisystem disease, congenital malformations, need for surgical intervention, and multi-disciplinary care needs.
Objective:
To determine the most commonly identified microorganisms and regional differences in blood stream infections (BSI) over the last 10 years within North American Level IV NICUs.
Design/Methods:
In this multi-center retrospective cohort study, clinical data from 39 North American Level IV NICUs within the Children’s Hospitals Neonatal Database (CHND) were analyzed. BSIs between January 2012 to December 2020 were identified. BSI was defined as the recovery of a bacterial pathogen from a blood culture with systemic signs of infection, and a minimum of 5 days of antimicrobial therapy for coagulase-negative Staphylococcus (CoNS). CHND Level IV sites were divided into zones based on geographic location (Figure 1). The relative frequency and regional distribution of the top 8 isolated microorganisms are described over the 10 year period.
Results:
The 10 year trend of the 8 most frequent organisms is displayed in figure 2. Among a total of 8,805 BSIs, CoNS decreased substantially from 43.2% of all treated organisms in 2012 to 27.5% in 2020. There was a comparative increase in Methicillin-sensitive Staphylococcus aureus (MSSA) (10.9% to 16.4%) and Escherichia coli (12.1% to 18.4%) over the decade. Across the 5 regions (figure 3), CoNS is least frequent in the Pacific (35%) compared to other regions (41-45% of culture positive BSIs). MSSA is less frequent in the North East (7%) versus the Pacific region (15%). Methicillin-resistant Staphylococcus aureus (MRSA) rates showed no regional difference (6-7% overall).
Conclusion(s):
CoNS infections declined across all Level IV NICU units nationally, contrasting with increasing proportion of E. coli and MSSA infections. Subtle geographical variations in microorganism distribution across CHND sites were identified. Describing the changing trends in reported culture positive causative organisms, and understanding regional variability is important for further hypothesis driven studies, and may guide clinical practice and antimicrobial stewardship efforts. 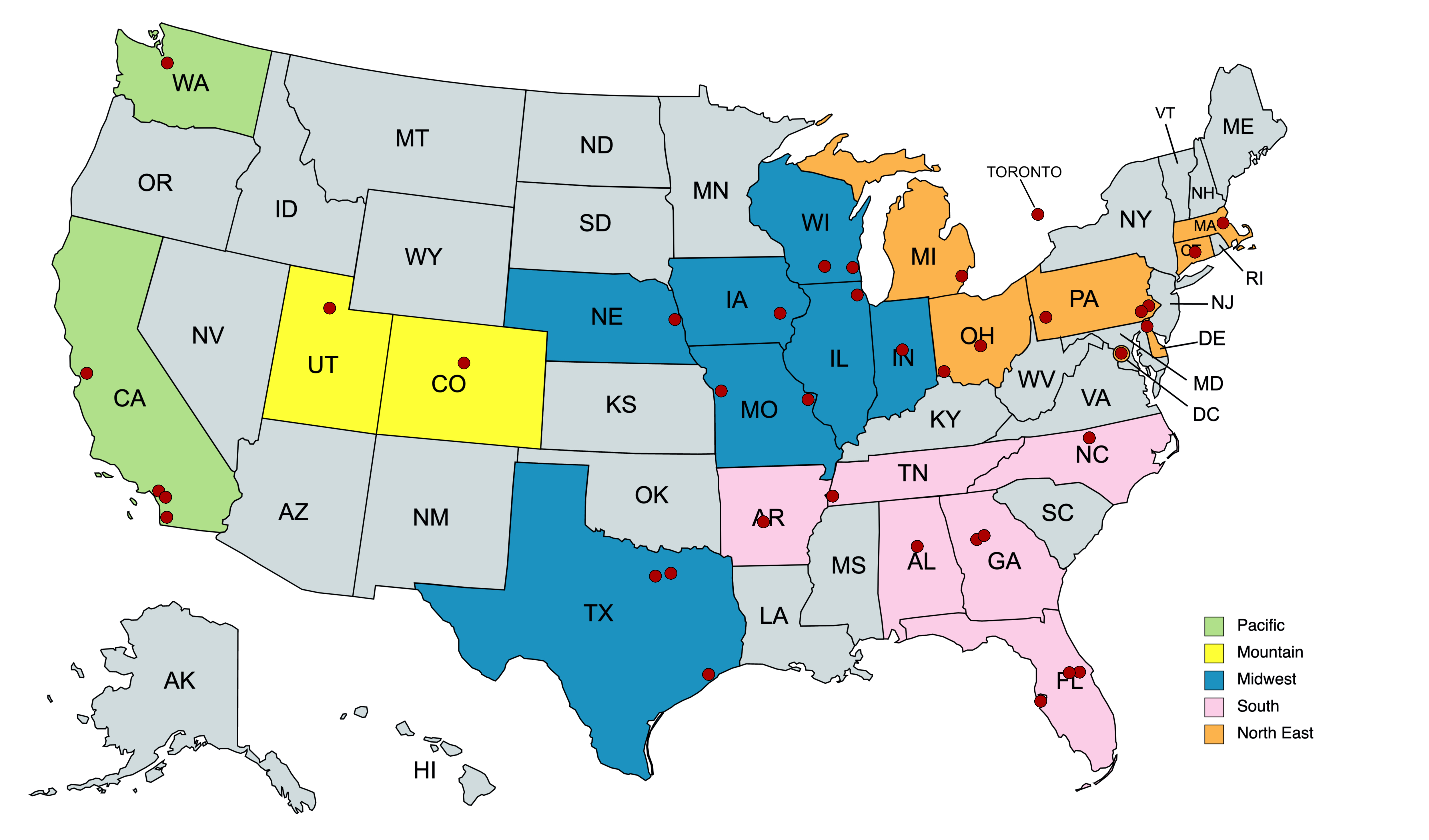
.jpg)
.jpg)
